Cardiology
(007) Concurrent Clozapine and Amiodarone Treatment

Jenna G. Bennett
Medical Student
Washington University School of Medicine
St. Louis, Missouri
Jenna G. Bennett
Medical Student
Washington University School of Medicine
St. Louis, Missouri
Can M. Kilciksiz, MD (he/him/his)
Clinical Assistant Professor
New York University School of Medicine
New York, New York
Can M. Kilciksiz, MD (he/him/his)
Clinical Assistant Professor
New York University School of Medicine
New York, New York
Tahir Rahman, MD, MD
Associate Professor
Washington University in St. Louis
SAINT LOUIS, Missouri
Tahir Rahman, MD, MD
Associate Professor
Washington University in St. Louis
SAINT LOUIS, Missouri
Presenting Author(s)
Co-Author(s)
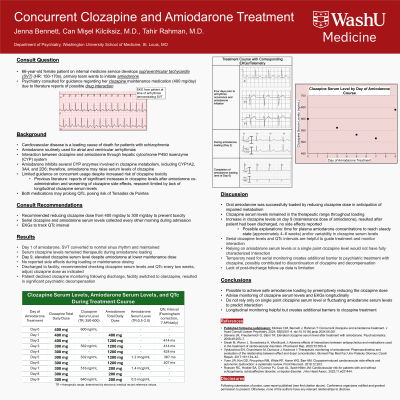
Background:
Amiodarone inhibits several cytochrome P450 enzymes involved in clozapine metabolism, but there is limited guidance on concurrent usage despite increased risk of clozapine toxicity (Stevens, 2008; Siwek, 2020). This interaction is important as cardiovascular disease is a leading cause of death for patients with schizophrenia (Rossom, 2022). To our knowledge, this is the only report with serial assays demonstrating amiodarone can be successfully loaded in the setting of clozapine maintenance treatment. A 66-year-old female with schizophrenia maintained on clozapine 400 mg/day was admitted to the internal medicine service for supraventricular tachycardia, necessitating amiodarone for the promotion of sinus rhythm. Psychiatry was consulted to provide guidance regarding potential drug interactions. We recommended reducing her clozapine dose from 400 mg/day to 300 mg/day to prevent toxicity after amiodarone initiation. Serial clozapine and amiodarone serum levels were then collected every other morning for one week, and EKGs were used to track QTc interval. Serum clozapine levels remained therapeutic during amiodarone loading. However, on the 3rd day following completion of the 6-day amiodarone load (day 9), the patient experienced an increase in clozapine serum levels despite a decreased clozapine dose and recent reduction of her amiodarone dose from loading to maintenance level. The patient did not experience any worsening clozapine side effects during hospitalization. The patient was discharged to her facility with recommendations to adjust clozapine dosage based on biweekly clozapine serum levels and EKG findings. Oral amiodarone was successfully loaded in this patient taking a maintenance dose of clozapine by reducing the clozapine dose in anticipation of its impaired metabolism. Clozapine serum levels remained in the therapeutic range throughout amiodarone loading, though then increased after 3 days on the lower maintenance dose of amiodarone. This may have occurred because plasma amiodarone concentrations take weeks to reach steady state (Vyskocilova, 2017). Therefore, we advise clinicians to monitor clozapine serum levels longitudinally, rather than relying on a single point clozapine serum level or fluctuating amiodarone serum levels, to predict the level of this highly dynamic interaction during or briefly after amiodarone loading. It is possible to achieve safe amiodarone loading in the setting of clozapine treatment by preemptively reducing the clozapine dose. Additionally, longitudinal serum clozapine levels and EKG monitoring may be helpful to adjust clozapine dosing and prevent toxicity during initiation of amiodarone treatment. Stevens JR, Freudenreich O, Stern TA. Elevated clozapine serum level after treatment with amiodarone. Psychosomatics. 2008;49(3):255–7. Siwek M, Woroń J, Gorostowicz A, Wordliczek J. Adverse effects of interactions between antipsychotics and medications used in the treatment of cardiovascular disorders. Pharmacol. Rep. 2020;72:350–9. Rossom RC, Hooker SA, O’Connor PJ, Crain AL, Sperl‐ Hillen JM. Cardiovascular risk for patients with and without schizophrenia, schizoaffective disorder, or bipolar disorder. J. Am. Heart Assoc. 2022;11(6):e021444. Vyskocilova EH, Grundmann M, Duricova J, Kacirova I. Therapeutic monitoring of amiodarone: Pharmacokinetics and evaluation of the relationship between effect and dose/concentration. Biomed. Pap. Med. Fac. Univ. Palacky Olomouc Czech Repub. 2017;161(2):134–43.
Case:
Results:
Discussion:
Conclusions:
References:
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: In addition to well-documented disparities in psychiatric care access and treatment, people of color are disproportionately impacted by cardiovascular disease. The cardiovascular health of women-identifying patients, such as ours, is also historically overlooked in both academic research and mainstream media. By sharing our experience treating a female patient with concurrent psychiatric illness and cardiovascular disease, a not uncommon combination, we hope to provide evidence-based guidance for providers in similar situations. Dissemination of such findings improves cardiovascular health, which again is disproportionately lower for people of color, and gives providers the confidence to appropriately and safely treat patients in need.

