Neurocognitive Disorders and Neuropsychiatry
(086) Anti-NMDAR Encephalitis, Ovarian Teratoma, and Psychosis: A Tangled Trio

Kimya Rod, MD (she/her/hers)
Resident Physician
Lincoln Medical and Mental Health Center
New York, New York- PR
Pronoy K. Roy, MD
Attending Physician
Lincoln Medical and Mental Health Center
Bronx, New York
Presenting Author(s)
Co-Author(s)
Background/Significance:
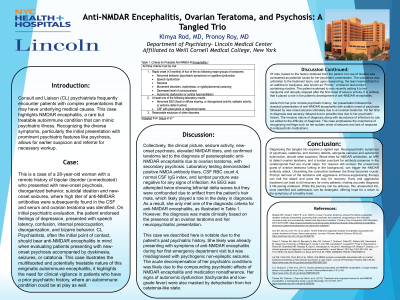
Consult and Liaison (CL) Psychiatrists frequently encounter patients with complex presentations that may have underlying medical causes. This case highlights anti-NMDAR encephalitis, a rare but treatable autoimmune condition that can mimic psychiatric illness. Recognizing the diverse symptoms, particularly the initial presentation with prominent psychiatric features like psychosis, allows for earlier suspicion and referral for necessary workup.
Case:
A 28-year-old woman with a remote history of bipolar disorder (unmedicated) who on initial psychiatric evaluation, presented with new-onset psychosis, endorsed feelings of depression, suicidal ideation, presented with speech latency, confusion, internal preoccupation, disorganization, and bizarre behavior. Along with new-onset seizures, where high titer of anti-NMDAR antibodies were subsequently found in the CSF and serum and ovarian teratoma was identified. CL Psychiatrists, often the initial point of contact, should bear anti-NMDAR encephalitis in mind when evaluating patients presenting with new-onset psychosis accompanied by dyskinesia, seizures, or catatonia. This case illustrates the multifaceted and potentially treatable nature of this enigmatic autoimmune encephalitis, it highlights the need for clinical vigilance in patients who have a prior psychiatric history, where an autoimmune condition could be at play as well.
Discussion:
Collectively, the clinical picture, seizure activity, new-onset psychosis, elevated NMDAR titers, and confirmed teratoma led to the diagnosis of paraneoplastic anti-NMDAR encephalitis due to ovarian teratoma, with secondary psychosis.
The acute decompensation was likely due to the compounding psychiatric effects of NMDAR encephalitis and medication nonadherence. Signs of autonomic dysfunction (tachycardia and low-grade fever) were also masked by dehydration from her catatonia-like state.
Her presentation followed the classical presentation of anti-NMDAR encephalitis with sudden onset of psychosis and new onset seizures ultimately due to an ovarian teratoma. Yet her time to diagnosis was delayed due to possible bias of prior psychiatric history. The invasive nature of diagnosis along with abundance of infections to rule out added to the difficulty of diagnosis. This case emphasizes the importance of recognizing red flags such as sudden onset of seizures and lack of response to antipsychotic medications.
Conclusion/Implications:
Diagnosing this tangled trio requires a vigilant eye. Neuropsychiatric symptoms of psychosis, catatonia, and memory deficits, alongside seizures and autonomic dysfunction, should raise suspicion. Blood tests for NMDAR antibodies, an MRI to detect ovarian teratoma, and a lumbar puncture for antibody presence in the cerebrospinal fluid are crucial steps. For reasons still unclear, ovarian teratoma can trigger the NMDAR antibody attack. Prompt removal of the teratoma and aggressive immune-suppressing therapy can halt the attack. Early treatment can lead to full recovery for many patients, making accurate diagnosis a life-saving endeavor. While the journey can be arduous, this unexpected trio, once identified, can be detangled, offering hope for return to the symphony of a healthy brain.
References:
Lai WS, Chan KW, Chan EW, et al. (2022). Anti-NMDA receptor encephalitis associated with an ovarian teratoma presenting as first-episode psychosis: a case report. Journal of Psychiatric Practice 28(1):84-88. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9987224/
Titulaer MJ, Dalmau J, Dopv de Ville A, et al. (2013). Treatment and prognostic factors for anti-NMDAR encephalitis: a retrospective study. Lancet Neurology 12(11):1067-1077. https://pubmed.ncbi.nlm.nih.gov/23290630/
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Time to diagnosis was delayed for this patient due to possible bias of being a woman with prior psychiatric history

