Psychopharmacology and Toxicology
(130) Allergic Reactions to Haloperidol: A Systematic Review

Kinza Tareen, MD
Clinical Assistant Profesor
University of Michigan
Ann Arbor, Michigan
Maureen Cassady, MD
Instructor
Brigham and Women's Hospital
Brookline, Massachusetts
Jordan H. Rosen, MD
Medical Director of Consultation-Liaison Psychiatry
University of Virginia
Charlottesville, Virginia
Presenting Author(s)
Co-Author(s)
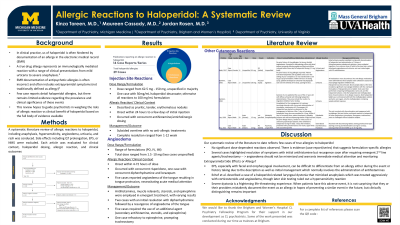
Background:
Haloperidol use in the hospital setting is ubiquitous, from the management to acute psychosis, agitation, emesis, to pain. As a result of its favorable pharmacokinetic profile, multiple routes of administration, and efficacy, haloperidol has gained favor as the most frequently used agent to treat delirium in the ICU.¹ Despite the evidence of its utility, in clinical practice, the use of haloperidol is often hindered by documentation of an allergy in the electronic medical record (EMR). A drug allergy represents an immunologically mediated reaction with a range of clinical presentations from mild urticaria to severe anaphylaxis.² The monitoring of adverse drug reactions is vital, however EMR documentation of antipsychotic allergies are often incorrect and often includes extrapyramidal symptoms not traditionally defined as allergy.³ Few case reports detail haloperidol allergies, but there remains limited evidence regarding the prevalence and clinical significance of these events. As such, we conducted a systematic review of the literature. In doing so, we aim to guide psychiatrists in weighing the risks of allergic reaction vs clinical benefit of haloperidol based on the full body of evidence available. A systematic review of literature was conducted per PRISMA guidelines. Three electronic databases (PubMed, Medline, and PsychInfo) were queried using keyword-based searches in March 2023. Article selection was limited to those that 1) described haloperidol in human subjects, 2) were published between 1958-February 2023, and 3) described any allergic reactions, including anaphylaxis, hypersensitivity, angioedema, urticaria, and rash. Side effects, including QT prolongation, TdP, dystonia, akathisia, parkinsonism, tardive dyskinesia, catatonia, or NMS were not included. 743 articles were initially identified through the three databases. 222 unique abstracts were identified, 177 articles were excluded, and 45 articles were screened in full. 14 articles met inclusion criteria. 14 articles reported an allergic reaction to haloperidol, of which 1 case of anaphylaxis was identified, 5 angioedema, 1 type IV hypersensitivity reaction, 1 urticaria, 3 rash, 1 injection site reaction, 1 generalized exanthematous pustulosis, and 1 case of photosensitive dermatitis. Discussion We plan to outline clinical presentations of haloperidol allergies, describe dystonic reactions that mimic allergic reactions, and propose an approach to stratifying the risk of documented haloperidol allergies. Implications: True allergic reactions attributed to haloperidol are exceedingly rare. Once known side effects relating to dopaminergic blockade were excluded, we found only case reports that support true allergy to haloperidol despite its widespread use for over half a century. This should be taken into account when weighing the risks and benefits of use when an unconfirmed haloperidol allergy is reported. Collet MO, Caballero J, Sonneville R, et al. Prevalence and risk factors related to haloperidol use for delirium in adult intensive care patients: the multinational AID-ICU inception cohort study. Intensive Care Med 2018;44:1081-1089. Thong BY, Leong KP, Tang CY, Chng HH. Drug allergy in a general hospital: Results of a novel prospective inpatient reporting system. Ann Allergy Asthma Immunol. 2003 Mar;90(3):342-7. Nurenberg JR, Schleifer SJ. Reported allergies to antipsychotic agents in a long-term psychiatric hospital. J Psychiatr Pract. 2009 Nov;15(6):489-92.
Methods:
Results:
References:
Presentation Eligibility: Not previously presented. We intend on submitting our work for publication in the future, but at the time of this submission, the manuscript is incomplete, and the probability of publication prior to November 2024 remains uncertain.
Diversity, Equity, and Inclusion: Despite the favorable safety profile of second-generation antipsychotics, racial disparities in the treatment of severe mental illness persist. African Americans are more likely than their white counterparts to be prescribed first-generation antipsychotics. Further, largely driven by cultural biases, marginalized groups are administered antipsychotics for agitation at a greater rate in the hospital setting. Unfortunately, this population is also at an increased risk for adverse drug reactions, including extrapyramidal symptoms, which are typically documented as an allergy. This presentation aims to broaden our understanding of documented allergies to haloperidol and stratify the risks associated with administering this commonly prescribed medication.

