Psychopharmacology and Toxicology
(129) Acute delirium caused by diphenhydramine withdrawal in a medically complex patient

Kate Warren, DO (she/her/hers)
PGY-4
Mount Sinai Beth Israel
New York, New York- SQ
Seema Quraishi, MD
Division Chief and Fellowship Program Director, Consultation-Liaison Psychiatry
Mount Sinai Beth Israel
New York, New York
Presenting Author(s)
Co-Author(s)
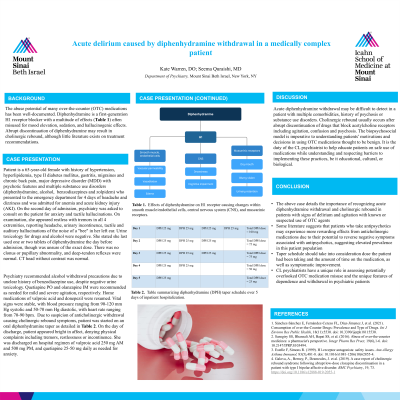
Background/significance: The abuse potential of many over-the-counter (OTC) medications has been well-documented (Sánchez-Sánchez, 2021). Diphenhydramine is a first-generation H1 receptor blocker often used for mood elevation, sedation, and hallucinogenic effects (Dose, 2000). Abrupt discontinuation of diphenhydramine may result in cholinergic rebound, although little literature exists on treatment recommendations. Psychiatry recommended alcohol withdrawal precautions due to unclear history of benzodiazepine use, despite negative urine toxicology. Olanzapine and quetiapine were recommended as needed for agitation. Home medications of valproic acid and donepezil were resumed. Vital signs were stable, with blood pressure ranging from 90-120 systolic and 50-70 diastolic, with heart rate ranging from 70-90. Due to suspicion of anticholinergic withdrawal causing cholinergic rebound symptoms, patient was started on an oral diphenhydramine taper and received 25 mg the first day, 25 mg x 3 the second and third day, 25 mg x 2 the fourth day, and 25 mg once the fifth day. On the day of discharge, patient appeared bright in affect, denying physical complaints including tremors, restlessness or incontinence. She was discharged on hospital regimen of valproic acid 250mg AM and 500mg PM, and quetiapine 25-50 mg daily as needed for anxiety.
Case: Patient is a 65 year old female with history of hypertension, hyperlipidemia, type II diabetes mellitus, gastritis, migraines and chronic back pain, major depressive disorder (MDD) with psychotic features and multiple substance use disorders (diphenhydramine, alcohol, benzodiazepines and zolpidem) who presented to the emergency department for 4 days of headache and dizziness and was admitted for anemia and acute kidney injury (AKI). On the second day of admission, psychiatry was asked to consult on the patient for anxiety and tactile hallucinations. On examination, she appeared restless with tremors in all 4 extremities, reporting headache, urinary incontinence, tactile and auditory hallucinations of the noise of a "bee" in her left ear. Urine toxicology for drugs and alcohol were negative. She stated she last used one or two tablets of diphenhydramine the day before admission, though was unsure of the exact dose. There was no clonus or pupillary abnormality, and deep-tendon reflexes were normal. CT head without contrast was normal.
Discussion: Acute diphenhydramine withdrawal may be difficult to detect in a patient with multiple comorbidities, history of psychosis or substance use disorders. Cholinergic rebound usually occurs after abrupt discontinuation of drugs that block acetylcholine receptors including agitation, confusion and psychosis (Galova, 2019). The biopsychosocial model is imperative to understanding patients’ motivations and decisions in using OTC medications thought to be benign. It is the duty of the CL psychiatrist to help educate patients on safe use of medications while understanding and respecting barriers to implementing these practices, be it educational, cultural, or biological.
Conclusion: The above case details the importance of recognizing and treating acute diphenhydramine withdrawal in patients with signs of delirium and agitation with known or suspected use of OTC agents, including diphenhydramine.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: This case report serves as a discussion of how socioeconomic factors and health literacy may impact
patients' understanding of the harms of over-the-counter medications, which have the potential for abuse. In a
different vein, as over-the-counter medications are easily accessible, this article seeks to challenge clinicians
to adapt the way they collect histories from patients in a way that does not impose judgement and equally
assesses all patients for substance misuse.

