Catatonia
(017) A Wolf in Cat’s Clothing: Amantadine in the treatment of SLE Catatonia

Hania Ibrahim, MD (she/her/hers)
Resident Physician
Duke University Hospital
Durham, North Carolina- MR
Michael Rauschenbach, MD PhD
Medical Resident
Duke University Med-Psych Program
Durham, North Carolina 
Oluwakemi M. Balogun, MD
Psychiatry Resident
Duke University Hospital Psychiatry Residency Program
DURHAM, North Carolina
Presenting Author(s)
Co-Author(s)
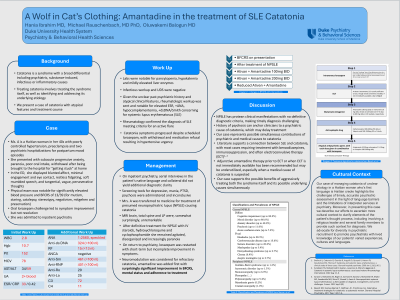
Background: Catatonia is a syndrome with a broad differential including psychiatric, substance-induced, infectious or inflammatory causes. Treating catatonia involves treating the syndrome itself, as well as identifying and addressing its underlying etiology. We present a case of catatonia with atypical features and treatment course. Case: Ms. A is a Haitian woman in her 40s with poorly controlled hypertension, preeclampsia and two psychiatric hospitalizations for postpartum mood episodes who presented with subacute progressive anxiety, paranoia, poor oral intake, withdrawal after being brought to the hospital for “getting stuck” at home. In the ED, she displayed blunted affect, minimal engagement and eye contact, restless fidgeting, soft mumbled speech, and tangential, vague, perseverative thoughts. Physical exam was notable for significantly elevated blood pressure and BFCRS of 13/39 (for mutism, staring, catalepsy, stereotypy, negativism, mitgehen and preservation). Oral lorazepam challenge led to symptom improvement but not resolution. She was admitted to inpatient psychiatry. Labs were notable for pancytopenia, hypokalemia and mildly elevated liver enzymes. Infectious workup and UDS were negative. Serial interviews in the patient’s native language and collateral did not yield additional diagnostic clarity. Screening tools for depression, mania, PTSD, psychosis were administered and inconclusive. Given the unclear past psychiatric history and atypical clinical features, rheumatologic workup was sent and notable for elevated ESR, +ANA, hypocomplementemia, +dsDNA/Smith concerning for systemic lupus erythematosus (SLE). Rheumatology confirmed the diagnosis of SLE meeting criteria for an active flare. Catatonia symptoms progressed despite scheduled lorazepam, with withdrawal and medication refusal resulting in hypertensive urgency. Mrs. A was transferred to medicine for treatment of presumed neuropsychiatric lupus (NPSLE) causing catatonia. MRI brain, total spine and LP were, somewhat surprisingly, unremarkable. After definitive treatment for NPSLE with IV steroids, hydroxychloroquine and cyclophosphamide she remained agitated, disorganized and increasingly paranoid. On return to psychiatry, lorazepam was restarted with short-term but incomplete improvement in symptoms, after which amantadine was added with surprisingly significant improvement in BFCRS, mental status and adherence to treatment. Discussion: Neuropsychiatric lupus (NPSLE) has protean clinical manifestations with no definitive diagnostic criteria, making timely diagnosis challenging. History of psychosis can anchor clinicians to a psychiatric cause of catatonia, which may delay treatment. Our case represents possible simultaneous contributions of psychiatric and medical causes to catatonia. Literature supports a connection between SLE and catatonia, with most cases requiring treatment with benzodiazepines, immunosuppression, and often electroconvulsive therapy (ECT) (Brelinksi, 2009; Sundaram, 2022). Adjunctive amantadine therapy prior to ECT or when ECT is not immediately available has been recommended but may be underutilized, especially when a medical cause of catatonia is suspected. Our case supports the possible benefits of aggressively treating both the syndrome itself and its possible underlying causes simultaneously. Brelinski L, Cottencin O, Guardia D, Anguill JD, Queyrel V, Hatron PY, Goudemand M, Thomas P. Catatonia and systemic lupus erythematosus: a clinical study of three cases. General hospital psychiatry. 2009 Jan 1;31(1):90-2. Sundaram TG, Muhammed H, Gupta L, Lawrence A, Misra R, Aggarwal A. Catatonia in systemic lupus erythematosus: case based review. Rheumatology International. 2022 Aug 1:1-6.
References:
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Our case of managing catatonia of unclear etiology in a Haitian woman who's first language is Haitian creole highlights the challenges of timely, accurate psychiatric assessment in the light of language barriers and the limitations of interpreter services in psychiatry. Moreover, in presenting this case we describe our efforts to ascertain more cultural context to clarify elements of the patient's thought process, including involving a religious leader and several family members to provide such context for diagnosis. We advocate for diversity in psychiatric recruitment to promote psychiatrists with lived knowledge of our patients' varied experiences, cultures and languages.

