Catatonia
(016) A Unique Intersection: A Case of Malignant Catatonia, PRES, and Cotard Delusions

Amy Y. Kim, BA
Medical Student
Rush Medical College
Chicago, Illinois- KR
Kelly Rhodes, MD
Assistant Professor
Rush University Medical Center
Chicago, Illinois
Presenting Author(s)
Co-Author(s)
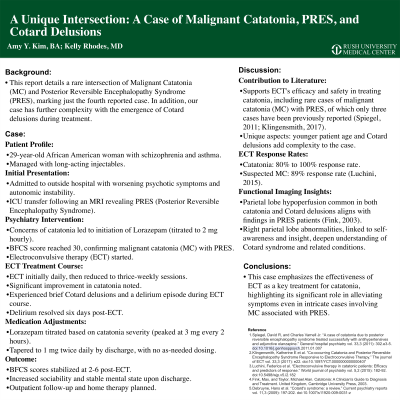
Background: This report details a rare intersection of Malignant Catatonia (MC) and Posterior Reversible Encephalopathy Syndrome (PRES), marking just the fourth reported case. In addition, our case has further complexity with the emergence of Cotard delusions during treatment.
Case: A 29-year-old African American woman with a history of schizophrenia and asthma, managed with monthly long-acting injectables, presented at an outside hospital with deteriorating psychotic symptoms, leading to progressive autonomic instability and necessitating an ICU transfer. An MRI revealed findings consistent with PRES, prompting her transfer to our NSICU. Concerns of catatonia led to a psychiatry consult and initiation of Lorazepam therapy, with dosages titrated to 2 mg hourly. Twelve hours later, her Bush-Francis Catatonia Rating Scale (BFCS) reached 30, leading to a diagnosis of MC in the context of PRES, and the commencement of electroconvulsive therapy (ECT).
ECT began daily, later shifting to thrice-weekly, showing significant catatonia improvement. After her 15th session, she briefly experienced Cotard delusions, believing she was dead and "in hell." A delirium spell occurred before her final, 18th session. Once ECT ended, her delirium resolved in six days.
Lorazepam was adjusted based on catatonia severity, peaking at 3 mg every two hours and titrated to 1 mg twice daily by discharge. Post-ECT, BFCS scores improved to 2-6. No as-needed Lorazepam was required. The patient displayed increased sociability, leading to her discharge with plans for outpatient follow-up and home therapy.
Discussion: This case adds to the literature confirming ECT's efficacy and safety in treating catatonia, even in cases of MC with PRES, of which only three other instances have been reported (Spiegel, 2011; Klingensmith, 2017). Our case, particularly marked by the youth of the patient and the presence of Cotard delusions, adds complexity. Studies show an 80% to 100% response rate to ECT in catatonia, increasing to 89% for suspected MC (Luchini, 2015). Functional imaging has revealed that parietal lobe hypoperfusion, a commonality between catatonia and Cotard delusions, matches findings in PRES patients (Fink, 2003). The link between Cotard delusions and abnormalities in the right parietal lobe, crucial for self-awareness and insight, broadens our understanding of these conditions.
Conclusion: This case emphasizes the effectiveness of ECT as a key treatment for catatonia, highlighting its significant role in alleviating symptoms even in intricate cases involving MC associated with PRES.
References:
- Spiegel, David R, and Charles Varnell Jr. “A case of catatonia due to posterior reversible encephalopathy syndrome treated successfully with antihypertensives and adjunctive olanzapine.” General hospital psychiatry vol. 33,3 (2011): 302.e3-5. doi:10.1016/j.genhosppsych.2011.01.007
- Klingensmith, Katherine E et al. “Co-occurring Catatonia and Posterior Reversible Encephalopathy Syndrome Responsive to Electroconvulsive Therapy.” The journal of ECT vol. 33,3 (2017): e22. doi:10.1097/YCT.0000000000000407
- Luchini, Federica et al. “Electroconvulsive therapy in catatonic patients: Efficacy and predictors of response.” World journal of psychiatry vol. 5,2 (2015): 182-92. doi:10.5498/wjp.v5.i2.182
- Fink, Max, and Taylor, Michael Alan. Catatonia: A Clinician's Guide to Diagnosis and Treatment. United Kingdom, Cambridge University Press, 2003.
- Debruyne, Hans et al. “Cotard's syndrome: a review.” Current psychiatry reports vol. 11,3 (2009): 197-202. doi:10.1007/s11920-009-0031-z
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Our case presentation reports on an African-American female, a member of a community often overlooked in medicine. It is important to continue advocating for equitable care for all genders and racial identities.

