Diversity, Equity, and Inclusion
(071) A Tale of Two Traumas: social determinants of health outcomes for patients with severe mental illness and traumatic brain injury, a case series

Leigh Berman, MD
Resident Physician
McGaw Medical Center of Northwestern University, Department of Psychiatry and Behavioral Sciences
Chicago, Illinois
Jason K. Onugha, MD, MPH (he/him/his)
Resident Physician
Northwestern University
Chicago, Illinois- VH
Veronika Hanko, MD
CL Psychiatrist
Northwestern University
Chicago, Illinois
Co-Author(s)
Presenting Author(s)
Co-Author(s)
Background
Severe mental illness (SMI) and traumatic brain injury (TBI) are closely associated, with TBI contributing to neuropsychiatric pathology and patients with psychiatric illness more likely to suffer TBI (Merrill, 2023). We present two cases of patients with SMI and TBIs to highlight psychosocial determinants leading to disparate outcomes.
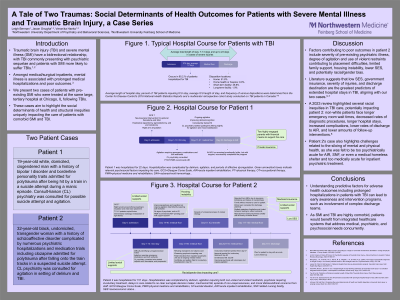
Case
Patient one is a 19-year-old white, domiciled, cisgendered man with a history of bipolar I disorder and borderline personality traits admitted to a tertiary care hospital for polytrauma after being hit by a train in a suicide attempt during a manic episode. On psychiatric evaluation, he exhibited intermittent agitation in setting of delirium and TBI requiring emergency medications and non-violent restraints. He started quetiapine 200mg nightly for mood stabilization and insomnia. The patient had two highly engaged parents with financial means to support his care. The patient improved medically and psychiatrically and was discharged to acute inpatient rehabilitation (AIR) after a 22-day medical hospitalization. At AIR, he remained emotionally labile, but with support, successfully completed the program.
Patient two is a 32-year-old black, undomiciled, transgender woman with a history of schizoaffective disorder admitted to the same hospital for polytrauma after falling onto the train tracks in a suspected suicide attempt. Psychiatry was consulted for agitation due to delirium and TBI and started valproic acid and olanzapine. She improved markedly from a neurologic standpoint, but AIR would not accept her without stable housing. Nursing homes declined her, citing her history of agitation—including use of violent restraints—and SMI. While awaiting placement, she became increasingly psychotic and medication nonadherent requiring court ordered involuntary treatment. Though her psychosis improved with psychotropics, her agitation continued due to TBI and frustration with prolonged hospitalization. The patient had limited family involvement or financial means to support her care. She was discharged to a shelter after a 151-day hospitalization.
Discussion
Factors contributing to poor outcomes in patient two included severity of TBI and pre-existing psychiatric illness, degree of agitation, use of violent restraints, limited family support, housing instability, lower socioeconomic status (SES), and potentially racial/gender bias. Literature demonstrates the impact of race/ethnicity, insurance, comorbid conditions including psychiatric illness, and SES on access to rehabilitation and long-term outcomes in TBI. As in our cases, lower SES is associated with longer hospital stays, and white patients are more likely to be discharged to inpatient rehabilitation than black patients (Johnson, 2023; Yue, 2023).
Conclusion
These cases—similar in presentation but vastly different in outcomes—highlight key social determinants impacting TBI patients’ care. As SMI and TBI are highly comorbid, patients would benefit from integrated healthcare systems that address medical, psychiatric, and psychosocial needs concurrently.
References
Merrill RM and Ashton MK. Rates of injury according to a single or comorbid mental illness identified in a large employee database. J Occup Health.2023;65(1):e12387.
Johnson LW and Diaz I. Exploring the social determinants of health and health disparities in traumatic brain injury: a scoping review. Brain Sci.2023;13(5):707.
Yue JK et al. Socioeconomic and clinical factors associated with prolonged hospital length of stay after traumatic brain injury. Injury.2023;54(9):110815.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: This presentation specifically focuses on inequities in care for patients with traumatic brain injuries. Using patient cases, we aim to examine the social determinants of health contributing to these inequities and advocate for systems level interventions to address them.

