Substance Use and Related Disorders
(164) A novel approach toward treating Fentanyl with Xylazine dependency

Nicholas Flugrad, MD (he/him/his)
Resident Physcian
Jersey Shore University Medical Center, Hackensack Meridian Health
neptune, New Jersey
Presenting Author(s)
Disclosure(s):
Nicholas Flugrad, MD: No financial relationships to disclose
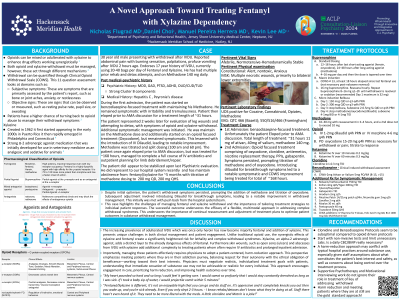
The convergence of opioid misuse and addiction has precipitated a dire public health crisis, with opioid-related deaths now surpassing those resulting from firearms and motor vehicle accidents in the United States [1]. Despite the high mortality rates associated with opioids, the prevalence of nonlethal overdoses is significantly greater, contributing substantially to the burden of opioid-related morbidity. Compounding this issue, approximately 80% of opioid overdoses involve polysubstance use, complicating both clinical management and public health responses [1,2].
The emergence of fully synthetic mu-opioid receptor agonists, notably fentanyl, has exacerbated the opioid crisis due to their heightened potency and widespread availability compared to traditional opioids like heroin [3]. The surge in fentanyl-related deaths has been exponential, with a staggering increase reported across multiple jurisdictions in recent years [4]. Simultaneously, the detection of xylazine-adulterated fentanyl, known as "tranq-dope," has also surged [5]. Xylazine, an alpha-2 adrenergic receptor agonist primarily used as a veterinary anesthetic, adds an additional layer of danger due to its combined use with fentanyl in human settings.
Management of withdrawal from fentanyl and xylazine presents significant challenges due to their potent pharmacological effects, including respiratory depression, sedation, hypotension, and the risk of tolerance and dependence. Previous benzodiazepine-focused treatment regimens have shown limited success, necessitating alternative approaches. Both governmental and scientific bodies have recognized fentanyl-xylazine combinations as a significant public health threat, acknowledging the lethal synergy between these drugs. Despite the growing evidence implicating xylazine in exacerbating fentanyl-related morbidity and mortality, comprehensive studies quantifying the interactions between these drugs remain scarce, underscoring the critical need for research to inform clinical practice and public health strategies aimed at mitigating the impact of this deadly drug combination.
Methods:
During a patient's previous admission for withdrawal, a benzodiazepine-focused treatment regimen was employed but proved ineffective. Subsequently, an opioid-focused approach was initiated, comprising oxycodone, clonidine, antiemetics, nicotine replacement therapy, proton pump inhibitors, and gabapentin. Methadone administration was delayed pending initial response assessment. Finally, a third option would have been employed if failure had been met with a focus on ketamine.
Discussion: Despite initial optimism, the patient's withdrawal symptoms persisted, prompting the addition of methadone and titration of oxycodone. Subsequent adjustment involved introducing Dilaudid for breakthrough symptoms, leading to a notable improvement in withdrawal management.
Conclusion/Implications: This case highlights the challenges of managing fentanyl and xylazine withdrawal and the importance of tailoring treatment strategies to individual patient responses. The successful outcome underscores the efficacy of a flexible, multimodal approach in addressing complex withdrawal syndromes. This underscores the importance of continual reassessment and adjustment of treatment plans to optimize patient outcomes in substance withdrawal management.
References:
1. Center forDiseaseControl,2023b. All Injury Mortality [WWW Document]. https://www.cdc.gov/nchs/fastats/injury.htm (accessed 3.4.24).
2. JonesCM,EinsteinEB,ComptonWM. Changes in Synthetic Opioid Involvement in Drug Overdose Deaths in the United States, 2010-2016. JAMA. 2018 May 1;319(17):1819-1821. doi: 10.1001/jama.2018.2844. PMID: 29715347; PMCID: PMC6583033.
3.GladdenRM,Martinez P,SethP.FentanylLawEnforcementSubmissionsandIncreases inSyntheticOpioid-InvolvedOverdoseDeaths-27States,2013-2014.MMWRMorbMortalWkly Rep.2016Aug 26;65(33):837-43.doi:10.15585/mmwr.mm6533a2.PMID:27560775.
4..National Institutes of Health, 2023. DrugOverdoseDeath Rates.[WWW Document].https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates (accessed 3.4.24).
5.United States Drug Enforcement Agency, 2023. DEA Reports Widespread Threat of Fentanyl MixedwithXylazine[WWW Document].https://www.dea.gov/alert/dea-reports-widespread-threat-fentanyl-mixed-xylazine (accessed 3.4.24).
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: This submission highlights the urgent need to address the opioid crisis, recognizing its disproportionate impact on historically marginalized communities. By emphasizing the challenges of managing withdrawal from fentanyl and xylazine and the limitations of current treatment approaches, it underscores the importance of developing more inclusive and effective strategies. Furthermore, by acknowledging the complexities of polysubstance use and the intersectional nature of opioid addiction, it promotes a more holistic understanding of the issue, which is essential for advancing diversity, equity, and inclusion in both research and clinical practice.

