Neurocognitive Disorders and Neuropsychiatry
(081) A Complex Journey through Misdiagnosis to Functional Neurological Disorder
.jpg)
Aliyeh Mahdavi Adeli, MD (she/her/hers)
Psychiatry Resident
Medical College of Georgia at Augusta University
Augusta, Georgia- AA
Argyro Athanasiadi, MD, MSc
Medical Director of Consultation and Liaison Psychiatry Department, Clinical Assistant Professor
Medical College of Georgia at Augusta University
Augusta, Georgia
Presenting Author(s)
Co-Author(s)
Background/Significance:
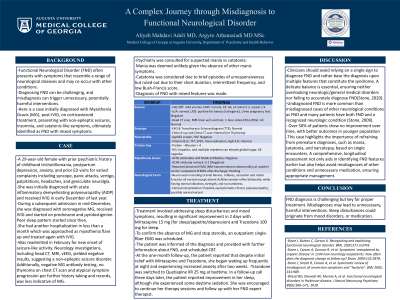
Functional Neurological Disorder (FND) often presents with symptoms that resemble a range of neurological diseases and may co-occur with other conditions. Diagnosing FND can be challenging and misdiagnosis can trigger unnecessary, potentially harmful interventions. Presented is a case initially diagnosed with Myasthenia Gravis (MG), post-IVIG, on corticosteroid treatment, presenting with non-epileptic seizures, insomnia, and catatonic-like symptoms, ultimately identified as FND with mixed symptoms.
Case:
A 29-year-old female with prior psychiatric history of childhood trichotillomania, postpartum depression, anxiety, and prior ED visits for varied complaints including syncope, panic attacks, vertigo, palpitations, headaches, and geniculate neuralgia. She was initially diagnosed with acute inflammatory demyelinating polyneuropathy (AIDP) and received IVIG in early December of last year. During a subsequent admission in mid-December, she was diagnosed with seronegative MG, received IVIG and started on prednisone and pyridostigmine. Poor sleep pattern started since then. She had another hospitalization in less than a month which was approached as myasthenia flare up and treated again with IVIG. Was readmitted in February for new onset of seizure-like activity. Neurology investigations, including head CT, MRI, vEEG, yielded negative results, suggesting a non-epileptic seizure disorder. Additionally, negative MG antibody testing, no thymoma on chest CT scan and atypical symptom progression per further history taking and records, was less indicative of MG. Psychiatry was consulted for suspected mania, though this was deemed unlikely given the absence of other manic symptoms. Catatonia was considered due to brief episodes of unresponsiveness but ruled out due to their short duration, intermittent frequency, and low Bush-Francis score. Diagnosis of FND with mixed features was made. Treatment involved addressing sleep disturbances and comorbidities, resulting in significant improvement in 2 days with Mirtazapine 15 mg and Trazodone 100 mg. To confirm the absence of MG and stop steroids an outpatient single-fiber EMG was scheduled. The patient was informed of the diagnosis and provided with further information about FND, and scheduled CBT.
Discussion:
Clinicians should avoid relying on a single sign to diagnose FND and rather base the diagnosis upon multiple features that constitute the syndrome. A delicate balance is essential, ensuring neither overlooking neurologic/general medical disorders nor failing to accurately diagnose FND(Stone, 2020). Undiagnosed FND is more common than misdiagnosed cases of other neurological conditions as FND and many patients have both FND and a recognized neurologic condition (Stone 2009). This case highlights the importance of refraining from premature diagnoses, such as mania, catatonia, and narcolepsy, based on single encounters. A comprehensive, longitudinal assessment not only aids in identifying FND features earlier but also helps avoid misdiagnoses of other conditions and unnecessary medication, ensuring appropriate management.
Conclusion:
FND diagnosis is challenging but key for proper treatment. Misdiagnoses may lead to unnecessary, harmful interventions. Sleep disturbances could originate from symptoms, comorbidities, or medication.
References:
-Stone J, Burton C, Carson A. Recognizing and explaining functional neurological disorder. BMJ. 2020;371:m3745.
-Stone J, Carson A, Duncan R, et al. Symptoms 'unexplained by organic disease' in 1144 new neurology outpatients: how often does the diagnosis change at follow-up? Brain. 2009;132:2878.
Presentation Eligibility: "Not previously published or presented"
Diversity, Equity, and Inclusion: Our speaker panel embodies diversity and inclusion, featuring a first-year IMG psychiatry resident of Middle Eastern descent currently in residency in Georgia, born in Germany, and mentored by an early career Consultation-Liaison attending who is also an international medical graduate from Greece. By highlighting a case involving a mixed-race young female and addressing misdiagnosis, we also shed light on the disparities experienced by women and racial and ethnic minorities in healthcare. This not only enhances our understanding of FND but also contributes to promoting diversity, equity, and inclusion within our professional community.

