Suicidality and Behavioral Emergencies
(178) A case report of concurrent mania and severe excoriation disorder resulting in skull osteomyelitis and pachymeningitis.

Deborah Benevenuto, MD (she/her/hers)
Psychiatrist
Advocate Aurora Health
Milwaukee, Wisconsin- EM
Elizabeth Meller, MD
Consultation-Liaison Psychiatrist
VA Boston
Boston, Massachusetts - EN
Eli S. Neustadter, MD, MSc
Psychiatry resident
Department of Psychiatry, Yale School of Medicine
New Haven, Connecticut 
Jennifer McMahon, MD
Assistant Professor of Psychiatry
Yale School of Medicine
New Haven, Connecticut
Presenting Author(s)
Co-Author(s)
BACKGROUND
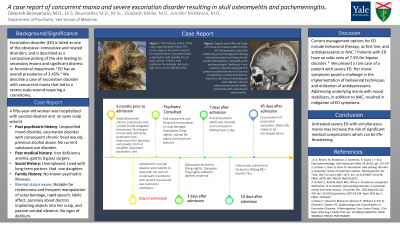
Excoriation disorder (ED) is listed as one of the obsessive–compulsive and related disorders, and is described as a compulsive picking of the skin leading to secondary lesions and significant distress or functional impairment (Brown,2015). ED has an overall prevalence of 3.45% (Farhat,2023). We describe a case of excoriation disorder with concurrent mania that led to a severe scalp wound requiring a craniotomy.
CASE REPORT
A fifty-year-old woman was hospitalized at Yale New Haven Hospital in September 2023 with suicidal ideation and an open purulent scalp wound. Her history is notable for iron deficiency anemia, gastric bypass surgery, mood disorder and excoriation disorder with consequent chronic head wound. Patient had been prescribed sertraline by her primary care provider although reported non-adherence at admission. She reported past heavy alcohol use and ongoing intermittent binge episodes. She denied drug use. She lived with a long-term partner, had a daughter, and was unemployed. Neuroimaging demonstrated pachymeningitis and osteomyelitis in the frontoparietal region underlying the open scalp wound. The patient underwent an uncomplicated craniotomy with wound closure and was started on antibiotics via peripheral inserted central catheter, which precluded transfer to inpatient psychiatry. Her initial mental status exam was significant for restlessness and frequent manipulation of scalp bandage, rapid speech, labile affect, paranoia about doctors implanting objects into her scalp, and passive suicidal ideation. Olanzapine was initiated and up-titrated to 30 mg total daily over two weeks and was associated with mild improvement. N-acetylcysteine (NAC) was started for ED, and the patient required 1:1 observation after attempted elopement and to minimize scalp manipulation. Lithium was eventually added, with improvement of manic symptoms, suicidal ideation and improved insight into her distrust of providers. She was discharged after five weeks with psychiatric follow-up and home visiting nurse services.
DISCUSSION
Current management options for ED include behavioral therapy, as first line, and antidepressants or NAC (Lochner,2017). Patients with ED have an odds ratio of 7.5% for bipolar disorder (Kwo,2020). We present a rare case of a patient with severe ED. Her manic symptoms posed a challenge in the implementation of behavioral techniques and utilization of antidepressants. Addressing underlying mania with mood stabilizers, in addition to NAC, resulted in mitigation of ED symptoms.
CONCLUSIONS
Untreated severe ED with simultaneous mania may increase the risk of significant medical complications which can be life-threatening.
REFERENCES
Brown GE, Malakouti M, Sorenson E, Gupta R, Koo JY. Psychodermatology. Adv Psychosom Med. 2015;34:123-34.doi:10.1159/000369090.Epub 2015 Mar 30. PMID: 25832518.
Farhat LC, Reid M, Bloch MH, Olfson E. Prevalence and gender distribution of excoriation (skin-picking) disorder: A systematic review and meta-analysis.J Psychiatr Res. 2023 May;161:412-418.doi:10.1016/j.jpsychires.2023.03.034. Epub 2023 Apr 1.PMID: 37023597.
Kwon C, Sutaria N, Khanna R, Almazan E, Williams K, Kim N, Elmariah S, Kwatra SG. Epidemiology and Comorbidities of Excoriation Disorder: A Retrospective Case-Control Study. J Clin Med. 2020 Aug 21;9(9):2703.doi: 10.3390/jcm9092703.PMID: 32825621; PMCID: PMC7564859.
Lochner C, Roos A, Stein DJ. Excoriation (skin-picking) disorder: a systematic review of treatment options. Neuropsychiatr Dis Treat. 2017 Jul 14;13:1867-1872.doi:10.2147/NDT.S121138. PMID: 28761349;PMCID: PMC5522672.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: As a Latina woman born and raised in Rio de Janeiro, Brazil, and currently pursuing consultation-liaison psychiatry fellowship at Yale University, my presence at the ACLP 2024 represents the diverse voices within psychiatry and underscores the importance of an inclusive representation. Through this poster presentation, I aim to foster empathy and awareness among my colleagues. By sharing my unique perspective and experiences, I highlight the importance of acknowledging and valuing the cultural diversity within our field. In doing so, I hope to inspire a shift towards more culturally competent and inclusive approaches to psychiatric care.

