Cardiology
(004) A Case of Duloxetine-Induced Hypotension in a Pediatric POTS Patient
- MF
Matthew Fiorillo, DO (he/him/his)
Child Psychiatry Fellow
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois - JW
Jonathon Wanta, MD
Assistant Professor
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois - MB
Moshe Bitterman, MD
Assistant Professor
Pritzker Department of Psychiatry and Behavioral Health
Chicago, Illinois
Co-Author(s)
Presenting Author(s)
Co-Author(s)
Background/Significance: Postural Tachycardia Syndrome (POTS) is a condition characterized by tachycardia without hypotension when transitioning to the upright position. Patients present with orthostatic intolerance, and may display symptoms concerning for somatization including palpitations, lightheadedness, weakness, and fatigue. Depression and anxiety are often associated with POTS, and so antidepressants are common treatment approaches. This case report involves a patient with POTS who experienced an adverse reaction to duloxetine.
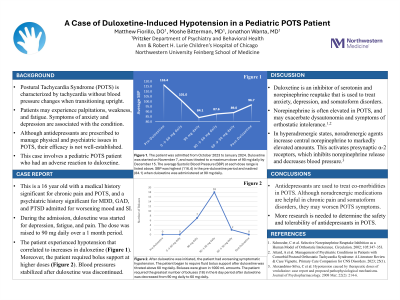
Case: The patient is a 16 year old adolescent with a past medical history significant for chronic pain and POTS, and a past psychiatric history significant for MDD, GAD, and PTSD who was admitted to the inpatient mental health unit for worsening mood and suicidal ideation. During the admission, duloxetine was started at 20 mg daily for mood, fatigue, and chronic pain. The dose was raised to 90 mg daily over the course of a month. The patient experienced symptomatic hypotension that corresponded to increases in duloxetine. Moreover, there was a clear correlation between duloxetine titration and SBP/DBP nadirs: 89/53 before duloxetine, 78/45 on 60 mg of duloxetine, and 59/30 on 90 mg of duloxetine. It is noteworthy that the patient required fluid boluses at higher doses of duloxetine. Atenolol, ivabradine, and midodrine were administered at various points in the treatment course, but no blood pressure changes were observed when these medications were either started or discontinued. Blood pressures only stabilized after duloxetine was discontinued.
Discussion: Duloxetine is an inhibitor of serotonin and norepinephrine reuptake. In addition to treating depression and anxiety, the medication is well-known to have benefit in somatoform disorders. The etiology of this effect is unclear, but is likely related to the segmental and suprasegmental desensitization of neurons that is mediated by norepinephrine. This same neurotransmitter may be involved in dysautonomia. In fact, some studies have demonstrated that excess norepinephrine can exacerbate orthostatic intolerance (Schroeder, 2002). In certain subtypes of POTS, particularly those where norepinephrine is already elevated, noradrenergic medications can produce an excessive central adrenergic response (Attard, 2023). At least one case report suggests that increased synaptic norepinephrine levels can stimulate presynaptic α-2 adrenergic receptors. This, in turn, reduces norepinephrine release from nerve terminals and can lower blood pressure (Alexandrino-Silva, 2008). This case study is important because it demonstrates that use of SNRIs or TCAs in hyperadrenergic states such as POTS can contribute to paradoxical hypotension.
Conclusion: Antidepressants are commonly used to treat psychiatric co-morbidities in POTS. Although SNRIs and TCAs can be an effective treatment in chronic pain and somatoform disorders, these medications may exacerbate POTS symptoms.
References:
1. Schroeder, C et al. Selective Norepinephrine Reuptake Inhibition as a Human Model of Orthostatic Intolerance. Circulation. 2002; 105:347–353.
2. Attard, A et al. Management of Psychiatric Conditions in Patients with Comorbid Postural Orthostatic Tachycardia Syndrome: A Literature Review and Case Vignette. Primary Care Companion for CNS Disorders. 2023; 25 (1).
3. Alexandrino-Silva, C et al. Hypotension caused by therapeutic doses of venlafaxine: case report and proposed pathophysiological mechanisms. Journal of Psychopharmacology. 2008 Mar; 22(2): 214-6.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Postural Orthostatic Tachycardia Syndrome (POTS) is a form of dysautonomia. Patients present with orthostatic intolerance, and may display symptoms concerning for somatization. This may lead to significant functional impairment, and can further worsen symptoms of anxiety and depression. To make matters worse, the underlying pathophysiology of the condition is poorly understood. Many providers simply dismiss POTS as a "mental health condition." This case report raises awareness for the disorder, and offers adverse reactions that can occur with noradrenergic medications (including SNRIs and TCAs).

