Women's Mental Health
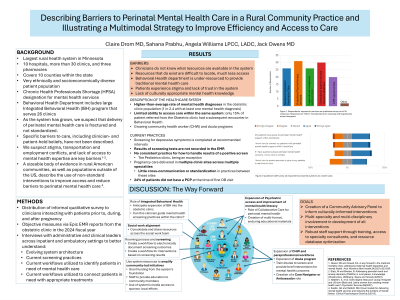
(225) Describing Barriers to Perinatal Mental Health Care in a Rural, Community Practice and Illustrating a Multimodal Strategy to Improve Efficiency and Access to Care

Claire Drom, MD (she/her/hers)
Staff Psychiatrist
CentraCare
St. Cloud, Minnesota
Sahana Prabhu, n/a
Medical Student
Dell Medical School
Flower Mound, Texas- AW
Angela Williams, LPCC, LADC
Psychotherapist
CentraCare St. Cloud Hospital
St. Cloud, Minnesota 
Jack Owens, MD
Staff Psychiatrist
Cleveland Clinic
Cleveland, Ohio
Presenting Author(s)
Co-Author(s)
Maternal mental health conditions are now implicated among the leading causes of death among women during pregnancy and in the first year postpartum. The majority of these deaths occur six to eight months following delivery, when most women are not regularly followed by a prescribed appointment schedule and their only point of contact with formalized healthcare may be through their child’s pediatrician (Minnesota Department of Health, 2020). Existing descriptive data suggests that living in rural settings in and of itself increases the risk of maternal mental illness due to limited access to transportation, technology, and childcare as well as increased reliance on maternal labor to earn income with inconsistent returns(Statz, 2023). In our large rural, non-academic healthcare system we believe the challenges in delivering timely access to direct and consultative psychiatric care are shared across systems through the United States.
Methods
In this project, we intend to describe the perceived and known systemic barriers to perinatal mental health care delivery within our system and within our community. We are distributing an informal, qualitative survey of clinicians interacting with patients prior to, during, and after pregnancy. This group includes practitioners in family medicine, obstetrics and gynecology, psychiatry and psychotherapy, and pediatrics. Using this survey data and objective metrics from the electronic medical record, we hope to more clearly define and describe the barriers to care within our system and communities. From this, we hope to illustrate a multimodal strategy for addressing gaps in care by utilizing consultative psychiatric models, as well as by training non-physician and non-psychiatric clinicians to disseminate information and treatment. Results and Discussion: In process We will describe the current flow of maternal mental health management through the system, including screening practices during and after pregnancy, the number of perinatal patients with and without established primary care providers at the 6-week postpartum obstetric visit, and the current practices by which we may identify a postpartum patient in need of mental health support. We will also present qualitative data from a staff survey. Discussion Prior to collecting survey data, we know that clinicians within our organization and within the community experience a general sense of frustration with access to care. We hypothesize this frustration in and of itself is a barrier to referrals to specialty mental health care. By gathering this data and describing the scope of the problem more clearly, we hope to move from an attitude of nebulous futility to hope for actionable change. We hope to illustrate a pathway to systemic and community change that is informed by perspectives of those who live and work within the context of the system. References Glazer, KB and Howell, EA. A way forward in the maternal mortality crisis: addressing maternal health disparities and mental health. Arch Womens Ment Health;24(2021):823-830. Minnesota Department of Health. (2020). Minnesota Maternal Mortality Report, 2017-2018. Statz, M and Bristow, B. Addressing perinatal mood and anxiety disorders (PMADs) in rural places: A knowledge infrastructure. Wellbeing, Space and Society;4(2023).
Presentation Eligibility: not previously published or presented
Diversity, Equity, and Inclusion: Inequities in social determinants of health are central to the experience of mental health symptoms and disorders in the perinatal period. Very little research has been done in the field of rural perinatal mental health, further marginalizing these under-served communities. This work focuses on bringing the same knowledge and standard of care to patients who are often neglected by traditional research methods and catchment areas.

