Collaborative and Integrated Care
(056) Depression and Anxiety Outcomes in Integrated Care at University of Connecticut Health Center

Ajit Deshpande, MD
Resident Physician
University of Connecticut
Farmington, Connecticut
Luis A. Velez, M.D
Resident Physician
University of Connecticut
HARTFORD, Connecticut- SK
Shakaib Khan, M.D
Assistant Professor
University of Connecticut
Farmington, Connecticut
Presenting Author(s)
Co-Author(s)
Background/Significance:
In Connecticut, the percentage of the population diagnosed with mental health disorders has increased overall since 2012. Between 2012–2017, the prevalence of depression, anxiety disorder, ADHD, and other mental disorders increased by 19%, 70%, 35%, and 34%, respectively. Notably, our state’s prevalence rates for these mental disorder categories exceeded the prevalence for the nation overall. We have been able to address the access issue and treat depression and anxiety with a short-term acute stabilization model.
Methods:
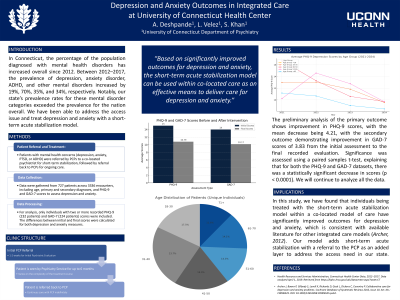
Patients with mental health concerns identified by PCP were referred by PCP to the co-located psychiatrist for short-term acute stabilization of depression, anxiety, PTSD, or ADHD with a referral back to PCP for continued treatment. IRB approval is currently accepted for an exempt study (24X-162-2). Electronic medical record data was extracted for patients in seven integrated care clinics from 8/5/2021 to 3/7/2024. A sample of data was collected from 727 patients over 3336 encounters. Data included age, primary diagnosis, and secondary diagnosis, along with the form of PHQ-9 and GAD-7 scores as objective measures for depression and anxiety, respectively.
Data was collected in a worksheet for each assessment, collated to group test scores by each individual, and sorted by date. Data points with only one score were filtered out, resulting in 232 individuals with two or more recorded PHQ-9 scores and 224 with two or more GAD-7 scores. The difference between the initial and final scores was calculated from these data sets.
Results:
The preliminary analysis of the primary outcome shows improvement in PHQ-9 scores, with the mean decrease being 4.21, with the secondary outcome demonstrating improvement in GAD-7 scores of 3.83 from the initial assessment to the final recorded evaluation. Significance was assessed using a paired samples t-test, explaining that for both the PHQ-9 and GAD-7 datasets, there was a statistically significant decrease in scores (p < 0.0001). We will continue to analyze all the data.
Discussion:
In this study, we have found that individuals being treated with the short-term acute stabilization model within a co-located model of care have significantly improved outcomes for depression and anxiety, which is consistent with available literature for other integrated care models (Archer, 2012). Our model adds short-term acute stabilization with a referral to the PCP as an added layer to address the access need in our state.
Conclusion/Implications:
The short-term acute stabilization model can be used within co-located care as an effective means to deliver care for depression and anxiety.
References:
Health Resources and Services Administration, Connecticut Health Center Data, 2012–2017. Data analyzed April 1, 2019. Retrieved from https://bphc.hrsa.gov/uds/datacenter.aspx?state=CT
Archer J, Bower P, Gilbody S, Lovell K, Richards D, Gask L, Dickens C, Coventry P. Collaborative care for depression and anxiety problems. Cochrane Database of Systematic Reviews 2012, Issue 10. Art. No.: CD006525. DOI: 10.1002/14651858.CD006525.pub2.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: We aim to advance mental health collaboration within primary care by demonstrating the efficacy of our integrated care model. Our ultimate goal is to advance mental healthcare in a holistic, inclusive way, conscious of the compounding barriers to care faced by those with intersectional identities. In this way, we strive to create a more equitable means of accessing psychiatric care at the systems level to ensure the overall wellness of our most marginalized populations.

