Child and Adolescent Psychiatry
(040) COVID-19 Pandemic’s Effect on Children and Catatonia: Analysis of an Inpatient Pediatric Unit and Consultation-Liaison Psychiatry Service

Rianna Chu
4th Year Medical Student
Loyola University Stritch School of Medicine
Maywood, Illinois- AR
Anne Marie J. Radzik, n/a
Medical Student
Loyola University Chicago Department of Psychiatry
Chicago, Indiana 
Emily Martinbianco, BS
Medical Student
Loyola University Stritch School of Medicine
Chicago, Illinois
Neha Nibber, n/a
Medical Student
Loyola University Chicago, Stritch School of Medicine
Oak Park, Illinois- DE
Doreen R. Elrad, BAS
MS4
Loyola University Chicago Stritch School of Medicine
Oak Park, Illinois 
Laila Hasnain, B.S.
Medical Student
Stritch School of Medicine
Maywood, Illinois- SV
Savannah Vetterly, n/a
Medical Student
Stritch School of Medicine
McDonald, Pennsylvania 
Rachel Bartnett, n/a
Medical Student
Loyola University Chicago
Chicago, Illinois
Akpene Sarah Agamah, MD, MPH, MBA
Resident Physician
Loyola University Medical Center
Chicago, Illinois
Theodote K. Pontikes, MD, DFAACAP, DFAPA, FACLP
Associate Professor, Stritch School of Medicine & Program Director, Psychiatry Residency
Loyola University Medical Center
Maywood, Illinois- EM
Edwin Meresh, MD, MPH, FACLP
Professor of Psychiatry
Loyola University Medical Center
Maywood, Illinois
Presenting Author(s)
Co-Author(s)
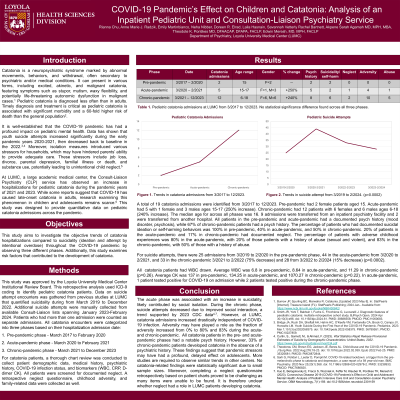
Background: Pediatric catatonia can be precipitated by fear and anxiety. At our center, there has been an increase in pediatric catatonia hospitalizations in the COVID-19 pandemic years of 2021 and 2023. There have been reports of COVID-19 as a stressor causing late onset catatonia in adults, however, there are no studies examining a similar phenomenon in children and adolescents1.This study aims to investigate the trends of catatonia hospitalizations compared to suicidality (ideation and attempt by intentional overdose) throughout the COVID-19 pandemic by observing three different phases.
Methods: This retrospective analysis used ICD-9 coding to identify pediatric catatonia and suicide attempt patients across three phases: 1. Pre-pandemic phase - March 2017 to February 2020, 2. Acute-pandemic phase - March 2020 to February 2021, 3. Chronic-pandemic phase - March 2021 to December 2023. Demographic data, medical history, COVID-19 infection status, biomarkers (WBC, CRP, D-dimer CK) were obtained. Data on suicide attempt was manually collected from available Consult-Liaison charts spanning 2022-2023. Data on any childhood adversity was obtained.
Results: Catatonia: pre-pandemic (n=2, female f=2, age 15), acute-pandemic (n=5, 250% increase, f=1, male m=3, age 15-17), and chronic pandemic (n=12, 240% increase, f=6, m=6, age 6-18).
Suicidality: pre-pandemic March 2019 – Feb 2020 (n=25), acute pandemic (n=44), and chronic pandemic March 2021 – February 2022 (n=33, 75% decrease) and March 2022 - February 2024 (n=28).
COVID-19 infection: acute-pandemic (n=1), chronic-pandemic (n=2).
All patients had WBC drawn. Average WBC: pre-pandemic (6.8), acute-pandemic (8.64), chronic-pandemic (11.29) (p=0.26). Average CK: pre-pandemic (137), acute-pandemic (134.25), chronic-pandemic (1070.27) (p=0.22)
Childhood adversity: 9 admissions were transferred from inpatient psychiatry facilities, 2 transferred from another hospital. 5 patients were ward of the state, 5 had cognitive delay (autism, ADHD, intellectual disability, learning disability), 3 had known neglect, 6 were victims of sexual and/or non-sexual abuse, 10 had parents with a notable psychiatric history.
Discussion: The acute phase was associated with an increase in suicidality, likely contributed by social isolation. During the chronic phase, intentional overdoses decreased due to improved social interaction, a trend supported by 2023 CDC data2. However, at LUMC, catatonia admissions increased drastically independent of COVID-19 infection. This suggests that the pandemic has had profound, delayed effects on adolescent mental health. Adversity may have contributed3.
Conclusion: The rise in pediatric catatonia cases at LUMC raises concern for the long-term impact of the pandemic. Pandemic stressors may have contributed to adversity. This finding highlights the need for accessible and consistent mental health services. More studies are required to observe similar trends in other centers during the chronic pandemic phase.
References: 1. Sarli G et al. COVID-19 related lockdown: a trigger from the pre-melancholic phase to catatonia and depression, a case report of a 59 year-old man. BMC Psychiatry. 2020 Nov 25;20(1):558.
2. Curtin, S et al. (2023). Vital Statistics Rapid Release Provisional Estimates of Suicide by Demographic Characteristics: United States, 2022. https://www.cdc.gov/nchs/data/vsrr/vsrr034.pdf
3. Dhossche DM et al. The role of deprivation, abuse, and trauma in pediatric catatonia without a clear medical cause. Acta Psychiatr Scand. 2012 Jan;125(1):25-32.
Presentation Eligibility: "Not previously published or presented"
Diversity, Equity, and Inclusion: COVID 19 pandemic affected children of low socioeconomic back ground.

