Suicidality and Behavioral Emergencies
(188) The Effect of QTc Prolongation on the Pharmacological Management of Behavioral Emergencies

Patrick Ying, MD, DFAPA
Assistant Professor of Psychiatry
NYU Grossman School of Medicine
New York, New York- RC
Rachel Caravella, MD (she/her/hers)
Director, CL Psychiatry Service
NYU Langone Health
BRIARCLIFF MANOR, New York - IG
Ilirjan Gjonbalaj, MD
Consultation-Liason Psychiatrist
NYU Langone Medical Center
New York, New York - AM
Abby Mulkeen, MD
Attending Psychiatrist, Consultation-Liaison Service
NYU Langone Health
New York, New York
Co-Author(s)
Presenting Author(s)
Co-Author(s)
The Effect of QTc Prolongation on the Pharmacological Management of Behavioral Emergencies
Background/Significance
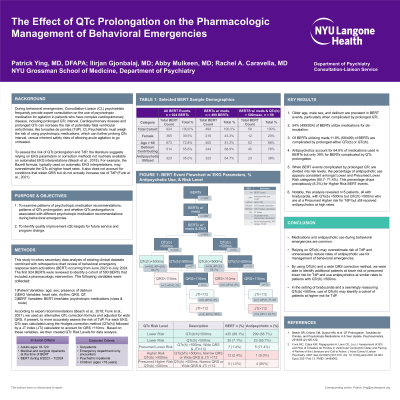
Consultation-Liaison (CL) psychiatrists frequently provide consultation for patients prescribed psychotropic medications who have complex cardiopulmonary disease, including prolonged QTc interval and risk for fatal ventricular arrhythmias, like torsades de pointes (TdP). During behavioral emergencies, CL Psychiatrists must weigh the risk of using psychotropic medications, which can further prolong QTc, versus allowing acute agitation to go untreated.
In order to assess the risk of certain psychotropic medications, the literature suggests relying on EKG parameters not routinely available on automated EKG interpretations. (Beach et al, 2018) For example, the Bazett formula can frequently overestimate the QTc interval at higher heart rates, while patients with conditions causing ventricular conduction delay leading to a widened QRS interval can also lead to a longer QTc interval without indicating increased risk of torsades de pointes. (Funk et al, 2021).
The Consultation-Liaison service at NYU Langone Health has developed tools to help more accurately calculate the QTc interval using the Hodges correction formula and as well as account for widened QRS intervals. This project seeks to identify how of QTc prolongation has affected the management of agitation during behavioral emergencies, and in particular, the frequency of these tools providing reassuring results after properly correcting for heart rate and widened QRS interval.
Methods
We reviewed 920 behavioral emergencies where the BERT team was activated for patients admitted to the NYU Langone Health over a 12 month period. We identified 533 events where pharmacological intervention was given. We will review these charts for QTc interval, the choice of pharmacological intervention, whether or not QTc interval affect the choice of prn medications, whether or not Hodges correction and/or adjustment for wide QRS was done in the setting of ventricular pacing or bundle branch block and whether that could or did affect the choice of prn medication.
Results
During these 533 behavioral emergencies, 388 patients received antipsychotic medications, 128 patients received benzodiazepines, 52 patients received valproate, 29 patients received medications in other categories (including non-benzodiazepine hypnotics, opioid and non-opioid pain medication and dexmetetomidine) Of the 145 patients that did not receive antipsychotic medication, 77 received benzodiazepines, 42 received valproate, and 27 patients received medications in other categories. Results will be presented as to frequency of apparent QTc prolongation with Bazett correction, persistent QTc prolongation after Hodges correction, or decreased concern for torsades de pointes after correction for widened QRS.
Discussion
These results will provide data about the frequency of prolonged or apparently prolonged QTc interval in the settings of behavioral emergencies over a one year period at a major academic medical center.
References
Beach SR, Celano CM, Sugrue AM, et al. QT Prolongation, Torsades de Pointes, and Psychotropic Medications: A 5-Year Update. Psychosomatics. 2018;59 (2):105-122.
Funk MC, Beach SR, Bostwick JR, et al. QTc Prolongation and Psychotropic Medications. Am J Psychiatry. 2020;177(3):273-274.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: This project seeks to help optimize the use of pharmacological therapies during behavioral emergencies in inpatient settings with patients with medical comorbidities. Previous research suggests that historically marginalized groups may have higher rates of behavioral emergencies, and higher rates of medical comorbidities.

