Training, Education, Mentorship, and Career Development
(202) Teaching Triaging: Case-Based Consultation-Liaison Psychiatry Workshop for Residents
.jpg)
Allison Rhodes, MD, MPH (she/her/hers)
Psychiatry Resident
Tufts Medical Center
Somerville, Massachusetts- VR
Varsha Radhakrishnan, MD
Consultation- Liaison Psychiatrist
Tufts Medical Center
Boston, Massachusetts - AN
Ashley Nieves - Archibald, MD (she/her/hers)
Consult-Liaison Attending Psychiatrist
Boston University School of Medicine
Boston, Massachusetts
Presenting Author(s)
Co-Author(s)
Lescinskas E, Sargsyan Z, Ayyala US, Fisher J. Preparing for Medical Internship: A Case-Based Strategy to Teach Management of Common Overnight Calls to Students. MedEdPORTAL. 2020;16:10966. https://doi.org/10.15766/mep_2374-8265.10966 Chen T, Stapleton S, Babcock M, Kelley MN, Frallicciardi A. Handoffs and Nurse Calls: Overnight Call Simulation for Fourth-Year Medical Students. MedEdPORTAL. 2021;17:11138. https://doi.org/10.15766/mep_2374-8265.11138
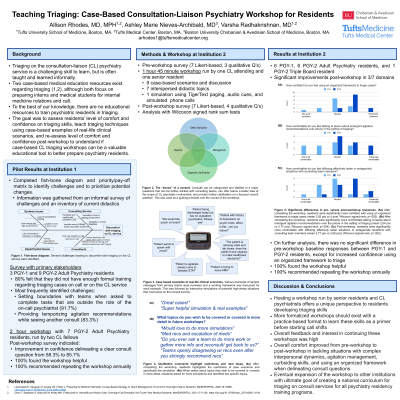
Background: Triaging on the consultation-liaison psychiatry service is a challenging skill to learn, but is often taught and learned informally. Two case-based medical education resources exist regarding triaging (Lescinskas, 2020; Chen, 2021), although both focus on preparing interns for internal medicine rotations and call. No education resources exist that we know of to train psychiatric residents in consultation triaging skills.
Methods: An informal survey of current challenges with triaging on the CL service was conducted at one academic institution with psychiatry residents, CL fellows, and attendings. Responses demonstrated a desire for more formal education in triaging, as well as an interest in practicing these skills through case-based examples and simulations. Based on this assessment, we implemented a QI pilot study focused on teaching triaging techniques through a case-based simulated workshop. PGY2 residents were identified as the highest yield population as residents would begin overnight CL/ED call shifts their PGY-3 year. Likert-scale based surveys were administered at the beginning and end of the workshop to assess comfort with calling teams to triage new consults, identifying a clear consult question, providing preliminary emergent agitation recommendations, navigating situations in which the consulting team disagrees with recommendations, curbsiding consults, and diffusing affectively laden or antagonistic situations with consulting teams. An updated version of this workshop will be implemented at another academic institution with IRB approval underway. Data will be analyzed pre and post workshop using surveys to assess the above triaging domains, and findings from both institutions will be available for presentation at this meeting.
Results: Preliminary analyses from the pilot study at the first institution demonstrate that participants had increased comfort and confidence across all triaging domains. In the pre-workshop survey, only 58.3% residents reported feeling very confident delineating a clear consult question, while in the post workshop survey 85.7% felt very confident. Results will be further analyzed based on years of training and across institutions. Qualitative feedback will also be collected, analyzed, and presented.
Discussion: From our pilot study, residents have qualitatively reported substantial benefit from the workshop in improving both confidence and preparedness for rotating on call and on the CL service, with interest in conducting and expanding upon simulation based learning for CL psychiatry. Pending final quantitative analysis at a different institution to assess generalizability of this intervention, we aim to further develop this workshop to ultimately build an adoptable triaging curriculum across all psychiatry residencies.
Conclusion: CL Triaging workshops through case based simulations can be a valuable educational tool to better prepare psychiatry residents on call and on the CL psychiatry service.
References:
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Triaging consults, communicating effectively with other teams, and managing conflicts are important skills that are often taught informally. This workshop aims to move these skills from the “hidden” or informal residency curriculum into the “explicit” or formal curriculum. This workshop will proactively reach resident learners prior to or early into their experiences with call and consultation-liaison service. This will benefit marginalized residents who are often disproportionately impacted by exclusion from the hidden curriculum of residency education. Our presenters have a diversity of knowledge and experience, with presenters of color, LGBTQ+ identity, and levels of training (resident, attending) at two institutions.

