Neurocognitive Disorders and Neuropsychiatry
(102) Tardive Dystonia and the Perils of Telehealth
- EM
Elizabeth Meller, MD
Consultation-Liaison Psychiatrist
VA Boston
Boston, Massachusetts 
Jennifer McMahon, MD
Assistant Professor of Psychiatry
Yale School of Medicine
New Haven, Connecticut
Presenting Author(s)
Co-Author(s)
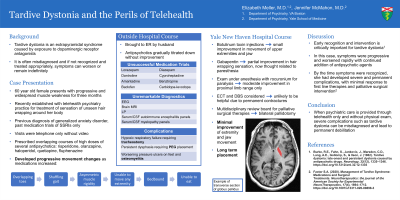
Background: Tardive dystonia is often misdiagnosed and can lead to permanent debilitation. We describe a case of tardive dystonia as a result of several months of escalating antipsychotic prescription through a telehealth-only practice, leading to severe complications and irreversible disability. Case: LB is a 60 year old female who presented with progressive and widespread muscle stiffness. She had recently established care with a telehealth psychiatry practice for treatment of sensation of unseen hair wrapping around her body. Over the course of three months, she had been prescribed overlapping courses of several antipsychotics, including risperidone, olanzapine, haloperidol, quetiapine, and fluphenazine. During this treatment, she began to develop movement changes, beginning with overlapping toes and progressing into shuffling gait and asymmetric muscle rigidity. There was no reduction in antipsychotics or treatment to ameliorate side effects, and her visits were via telephone only without video. She eventually developed inability to move all extremities, was bedbound, and eating minimally due to difficulty opening her mouth; she was subsequently admitted for inpatient treatment. Medication trials including standing lorazepam, dantrolene, cyproheptadine, amantadine, benztropine, baclofen, carbidopa-levodopa, and diazepam were attempted without improvement. Work-up including EEG, brain MRI, LP, and autoimmune encephalitis and myelopathy panels was unremarkable. Her course was complicated by hypoxic respiratory failure requiring tracheostomy, persistent dysphagia requiring PEG placement, and worsening pressure ulcers on her feet with development of osteomyelitis. She was transferred to Yale New Haven Hospital for specialty services and diagnosed with tardive dystonia. Botulinum toxin injections were completed with small improvement in movement of her upper extremities and jaw. Her sensation of hair wrapping was thought to be due to parasthesias and improved with standing gabapentin. She was examined under anesthesia to assess for development of permanent contractures; after paralysis with rocuronium, she had moderate improvement in proximal limb range of motion only. ECT was considered but determined to be unlikely to be beneficial. Her case was presented to a multidisciplinary review board for palliative surgical therapies with eventual decision to pursue bilateral pallidotomy. Several months after her surgery, she had minimal improvement in ability to move her extremities and jaw, with plan for long term care placement. Discussion: Early recognition and intervention is critically important for tardive dystonia (Burke, 1982). In this case, her symptoms were progressive and worsened rapidly with continued addition of antipsychotic agents; by the time her symptoms were recognized, she had developed several severe complications including permanent contractures and had minimal response to first line therapies and palliative surgical intervention (Factor, 2020). Conclusion: When psychiatric care is provided through telehealth only, severe complications such as tardive dystonia can be misdiagnosed and lead to permanent debilitation. 1. Burke, R.E., Fahn, S., Jankovic, J., Marsden, C.D., Lang, A.E., Gollomp, S., & Ilson, J. (1982). Tardive dystonia: late-onset and persistent dystonia caused by antipsychotic drugs. Neurology, 32(12), 1335–1346. https://doi.org/10.1212/wnl.32.12.1335 2. Factor S.A. (2020). Management of Tardive Syndrome: Medications and Surgical Treatments. Neurotherapeutics: the journal of the American Society for Experimental NeuroTherapeutics, 17(4), 1694–1712. https://doi.org/10.1007/s13311-020-00898-3
References:
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Not applicable

