Psychopharmacology and Toxicology
(149) Tardive Dyskinesia Improved by Lithium: A Case Report and Brief Literature Review
.jpg)
Tamar Jacobsohn, BA
Medical Student
NYU Grossman Long Island School of Medicine
NYC, New York
Alice Gelman, M.S.
Student
NYU Grossman
Mineola, New York
Aaron Pinkhasov, DFAPA, FACLP
Chairman, Department Of Psychiatry NYU Langone Hospital—Long Island Professor of Psychiatry and Med
NYU Langone Hospital—Long Island
Mineola, New York
Presenting Author(s)
Co-Author(s)
Background:
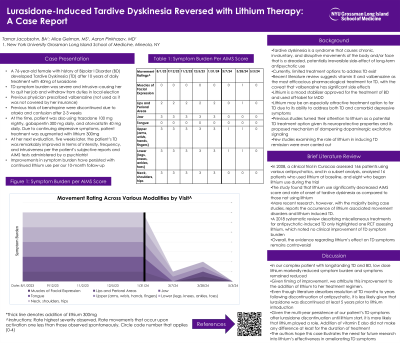
Tardive dyskinesia (TD) is a syndrome that causes chronic, involuntary movements of the body and/or face. It is a dreaded and potentially irreversible side-effect of long-term antipsychotic use. TD has a negative impact on quality of life and may precipitate social withdrawal (1). There are currently limited treatment options for TD and existing treatments fail to completely eliminate symptoms (2). Here, we review the literature discussing the interplay between lithium and TD and present a case report of TD improvement after lithium addition for treatment resistant depression. A 76-year-old female with diagnosis of Bipolar II Disorder (BD) developed TD after being treated with lurasidone for ten years that persisted after discontinuation. The patient’s depression did not respond to trials of bupropion and TMS. Lithium 300 mg per day was started to augment bupropion. At her five week follow-up visit, the patient’s TD was significantly improved based on subjective reports and AIMS scores. Given the potential neuroprotective effects of lithium, (3) and its proposed mechanism of dampening dopaminergic excitatory signaling (4), lithium may have promise in reduction of TD. Our literature review yielded two small clinical trials of 24 and 6 patients, respectively, that showed improvement of TD symptoms with lithium (5, 6). Recent case studies, however, suggest lithium may worsen or even cause TD symptoms (7, 8) and a 2011 systematic review describing treatments for antipsychotic-induced TD highlighted one RCT assessing lithium, which noted no clinical improvement (9). Thus, lithium’s role in TD treatment remains controversial. This case report aims to help to reinvigorate interest in lithium as a treatment agent for TD symptoms. More research is needed to revisit the potential role of lithium in TD amelioration. McEvoy J et al. Effect of tardive dyskinesia on quality of life in patients with bipolar disorder, major depressive disorder, and schizophrenia. Qual Life Res. 2019 Dec;28(12):3303-3312. doi: 10.1007/s11136-019-02269-8. Testini P and Factor SA (2023), Treatment of tardive dystonia: A review. Dystonia 2:10957. doi: 10.3389/dyst.2023.10957 Malhi GS et al. Potential mechanisms of action of lithium in bipolar disorder. Current understanding. CNS Drugs. 2013 Feb;27(2):135-53. doi: 10.1007/s40263-013-0039-0. Diniz BS et al. Lithium and neuroprotection: translational evidence and implications for the treatment of neuropsychiatric disorders. Neuropsychiatr Dis Treat. 2013;9:493-500. doi: 10.2147/NDT.S33086. van Harten PN et al. Evidence that lithium protects against tardive dyskinesia: the Curaçao Extrapyramidal syndromes study VI. Eur Neuropsychopharmacol. 2008 Feb;18(2):152-5. doi: 10.1016/j.euroneuro.2007.07.004. Reda FA et al. Lithium carbonate in the treatment of tardive dyskinesia. Am J Psychiatry. 1975 May;132(5):560-2. doi: 10.1176/ajp.132.5.560. Chakrabarti S, Chand PK. Lithium - induced tardive dystonia. Neurol India. 2002 Dec;50(4):473-5. PMID: 12577099. Akkus M. A case of dose-dependent lithium-induced tardive dyskinesia. J Affect Disord. 2022 Feb 15;299:205-20`6. doi: 10.1016/j.jad.2021.12.003. Epub 2021 Dec 4. PMID: 34871639. Soares-Weiser, K et al. (2018). Miscellaneous treatments for antipsychotic-induced tardive dyskinesia. The Cochrane database of systematic reviews, 3(3), CD000208. https://doi.org/10.1002/14651858.CD000208.pub2
Case:
Discussion:
Conclusion/Implications:
References:
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Our case report may help expand treatment options for patient suffering from psychiatric illness, many of whom have multiple comorbidities, necessitating the use multiple medications with burdensome long-term side effects. Our case report targets a syndrome that currently has no definitive treatment and may provide a new avenue of treatment to psychiatric patients for whom traditional treatments are contraindicated to drug interactions with medications taken for comorbid conditions.

