Neurocognitive Disorders and Neuropsychiatry
(101) Taming the Aftermath: Practical Approaches to Postictal Behavioral Management
- MS
Manuel Seraydarian, Pharm.D. (he/him/his)
Psychiatric Clinical Pharmacy Specialist
Memorial Regional Hospital
Hollywood, Florida - MS
Manuel Seraydarian, Pharm.D. (he/him/his)
Psychiatric Clinical Pharmacy Specialist
Memorial Regional Hospital
Hollywood, Florida 
Omair H. Abbasi, MD, FAPA, FACLP
Program Director
Memorial Healthcare System
Hollywood, Florida
Omair H. Abbasi, MD, FAPA, FACLP
Program Director
Memorial Healthcare System
Hollywood, Florida- AR
Alejandro Rodulfo, MD
Consultation Liaison Psychiatrist
Memorial Healthcare System
Hollywood, Florida - AR
Alejandro Rodulfo, MD
Consultation Liaison Psychiatrist
Memorial Healthcare System
Hollywood, Florida - AA
Alberto Augsten, PHARMD, DABAT
Director PGY2 Psychiatric Pharmacy Residency
NOVA Southeastern University
Hollywood, Florida - AA
Alberto Augsten, PHARMD, DABAT
Director PGY2 Psychiatric Pharmacy Residency
NOVA Southeastern University
Hollywood, Florida 
Daniel M. Pearlman, MD
Resident
Memorial Healthcare System
Coral Springs, Florida
Daniel M. Pearlman, MD
Resident
Memorial Healthcare System
Coral Springs, Florida- MZ
Mohammed Zakaria, MD
Chief, Neurology program
Memorial hospital
Plantation, Florida - MZ
Mohammed Zakaria, MD
Chief, Neurology program
Memorial hospital
Plantation, Florida
Presenting Author(s)
Co-Author(s)
Background/Significance:
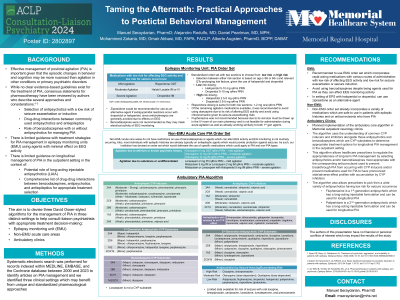
Effective treatments for the management of postictal agitation is important given the prevalence in persons with epilepsy (Subota, 2019). The episodic changes in behavior and cognition can occur in a variety of settings, leading to safety concerns for the patients themselves and others. Frequently, psychiatrists may be consulted to manage such symptoms, however the delineation of management strategies may be more nuanced than agitation seen in other conditions or primary psychiatric disorders. While no clear evidence-based guidelines exist for the treatment of postictal agitation, consensus statements for pharmacotherapy have been reviewed by authors who describe several approaches and considerations. These include selection of antipsychotics with a lower risk of inducing seizures, drug-drug interactions with antiepileptics, when to use oral or intramuscular routes of administration, and the role of benzodiazepines with or without antipsychotics for managing mild-moderate-severe conditions (Alper, 2002; Adachi, 2013; de Toffol, 2018). These reviews are largely based on applying the treatments used in primary psychotic conditions to epilepsy-associated behavioral conditions, given the sparsity of controlled studies in treating psychosis and agitation in persons with epilepsy. The aim of this submission is to devise three David Osser-styled algorithms for the management of postictal behavioral presentations in three distinct settings to help consult-liaison psychiatrists with timely treatment decision-making when such situations arise.
Methods:
We performed a systematic electronic search for records indexed within MEDLINE, EMBASE, and the Cochrane database between 2000 and 2023 to identify articles on postictal agitation management. We sought clinical trials, meta-analyses, randomized controlled trials, reviews, and systematic reviews. We manually reviewed the reference lists of qualified studies for further evidence. We identified three clinical settings that can benefit from unique and standardized pharmacological approaches from which to build on existing literature: epilepsy monitoring units (EMU), non-EMU acute care areas, and ambulatory care clinics.
Results:
Literature review is currently underway.
Discussion:
Discussion will be completed pending finalization of results.
Conclusion/Implications:
To be determined based on conclusion of the results. Our hope is to put forth a safe and effective framework for the timely management of postictal agitation in a variety of settings.
References:
Subota A, Khan S, Josephson CB, et al. Signs and symptoms of the postictal period in epilepsy: A systematic review and meta-analysis. Epilepsy Behav. 2019;94:243-251. doi:10.1016/j.yebeh.2019.03.014
Alper KR, Barry JJ, Balabanov AJ. Treatment of psychosis, aggression, and irritability in patients with epilepsy. Epilepsy Behav. 2002;3(5S):13-18. doi:10.1016/s1525-5069(02)00500-5
Adachi N, Kanemoto K, de Toffol B, et al. Basic treatment principles for psychotic disorders in patients with epilepsy. Epilepsia. 2013;54 Suppl 1:19-33. doi:10.1111/epi.12102
de Toffol B, Trimble M, Hesdorffer DC, et al. Pharmacotherapy in patients with epilepsy and psychosis. Epilepsy Behav. 2018;88:54-60. doi:10.1016/j.yebeh.2018.09.001
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: The results from this research can provide more direct guidance on the treatment of post-ictal agitation in marginalized groups historically initially treated with more aggressive medication management than non-marginalized groups.

