Catatonia
(032) Stuck at the Scene: Trauma-Emergent Catatonia in a Patient with Landau-Kleffner Syndrome

Linda Herrera Santos, MD, PhD (she/her/hers)
Attending Psychiatrist
Massachusetts General Hospital
Boston , Massachusetts- ES
Emily Sorg, MD
Psychiatrist
Massachusetts General Hospital
Boston, Massachusetts 
Jasmine Outlaw, MD
Physician
Massachusetts General Hospital
Everett, Massachusetts
Felicia A. Smith, MD (she/her/hers)
Associate Chief of Psychiatry, MGH
MGH
Boston, Massachusetts
Presenting Author(s)
Co-Author(s)
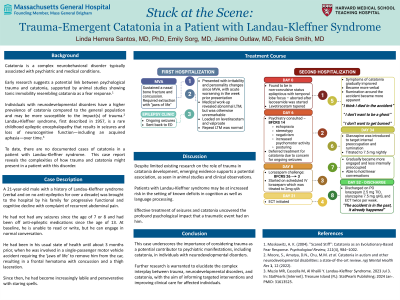
Background/Significance: Catatonia is a complex neurobehavioral disorder typically associated with psychiatric and medical conditions. Emerging research suggests a potential link between psychological trauma and catatonia, supported by animal studies showing tonic immobility resembling catatonia as a fear response (Moskowitz, 2004). Individuals with neurodevelopmental disorders have a higher prevalence of catatonia compared to the general population and may be more susceptible to the impact(s) of trauma (Moore, 2022). Landau-Kleffner syndrome, first described in 1957, is a rare childhood epileptic encephalopathy that results in seizures and loss of neurocognitive function—including acquired aphasia—over time. To date, there are no documented cases of catatonia in patients with Landau-Kleffner syndrome. This case report reveals the complexities of how trauma and catatonia might present in a patient with this disorder.
Case: A 21-year-old male with a history of Landau-Kleffner syndrome (verbal and on no anti-epileptics for over a decade) presented with his family for progressive functional and cognitive. He had been in his usual state of health until about 3 months prior, when he was involved in a motor vehicle accident requiring the ‘jaws of life’ to remove him from the car, resulting in a frontal hematoma with concussion. Since then, he had become increasingly labile, perseverative, and experienced staring spells. Medical work-up revealed non-convulsive status epilepticus with temporal focus prompting admission for seizure control but was otherwise unremarkable (including for autoimmune encephalitis). On psychiatric evaluation, he demonstrated prominent catatonic features, including echopraxia, posturing, stereotypy, negativism, and purposeless psychomotor activity that persisted well beyond seizure control. He was visibly distressed and perseverative, often repeating vague, guilty, or fearful phrases. Catatonia symptoms eventually responded to a combination of high-dose lorazepam and electroconvulsive therapy. As he became more verbal, rumination specifically around the accident became more apparent: “I think I died in the accident,” “I don’t want to be a ghost.” Olanzapine was added to aid internal preoccupation around the accident, resulting in a notable improvement in mood and engagement. At the time of discharge, he was euthymic, verbal, and linear with a newfound perspective that the “accident was in the past.” Outpatient follow-up notes indicate sustained improvement.
Discussion: This case underscores the importance of considering trauma as a potential contributor to psychiatric manifestations, including catatonia, in individuals with neurodevelopmental disorders. Despite limited existing research on the role of trauma in catatonia, emerging evidence supports a potential association. Patients with Landau-Kleffner syndrome may be at increased risk in the setting of known deficits in cognition and language processing. Effective treatment of seizures and catatonia uncovered the profound psychological impact that the traumatic event had on him. Further research is warranted to elucidate the complex interplay between trauma, neurodevelopmental disorders, and catatonia to inform targeted interventions and improve clinical care for affected individuals.
References:
Moskowitz, A. K. (2004). "Scared Stiff": Catatonia as an Evolutionary-Based Fear Response. Psychological Review, 111(4), 984–1002.
Moore, S., Amatya, D.N., Chu, M.M. et al. Catatonia in autism and other neurodevelopmental disabilities: a state-of-the-art review. npj Mental Health Res 1, 12 (2022).
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: This case underscores the distinctive role of CL psychiatry in navigating the clinical complexities encountered by patients with neurodevelopmental disorders, a population that has historically endured discrimination and healthcare inequities. It highlights the imperative to recognize and address the psychological impact of trauma, a facet often overlooked in individuals with communication and processing difficulties. By spotlighting this case, it advocates for healthcare providers to embrace a more inclusive and comprehensive approach to care, ensuring that the unique needs and experiences of this patient population are fully acknowledged and addressed.

