Psychopharmacology and Toxicology
(142) Integrative Care - A Novel Case of Paliperidone-Induced DRESS Syndrome

Nishant V. Surapaneni, M.S. - Biotechnology & Pharmacokinetics
Medical Student
Northeast Ohio Medical University (NEOMED)
Cleveland, Ohio
Nishant V. Surapaneni, M.S. - Biotechnology & Pharmacokinetics
Medical Student
Northeast Ohio Medical University (NEOMED)
Cleveland, Ohio
Alexander C. Mittman, MD
Resident
Case Western Reserve University / University Hospitals
Cleveland, Ohio
Alexander C. Mittman, MD
Resident
Case Western Reserve University / University Hospitals
Cleveland, Ohio
Jennifer Brandstetter, MD, FAPA
Assistant Professor
University Hospitals Cleveland Medical Center
Cleveland, Ohio
Jennifer Brandstetter, MD, FAPA
Assistant Professor
University Hospitals Cleveland Medical Center
Cleveland, Ohio
Syed Amir Z. Shah, MD
Attending
University Hospitals Cleveland Medical Center
Cleveland, Ohio
Syed Amir Z. Shah, MD
Attending
University Hospitals Cleveland Medical Center
Cleveland, Ohio
Presenting Author(s)
Co-Author(s)
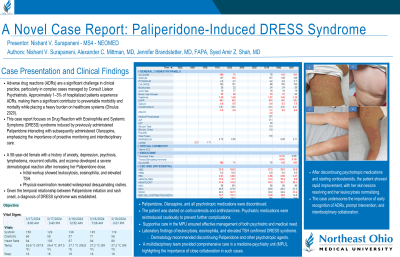
Background/Significance:
Adverse drug reactions (ADRs) are common concerns encountered in the clinical setting by Consult Liaison Psychiatrists. Affecting 1–3% of hospitalized patients, ADRs cause significant morbidity and mortality and place substantial burden on the healthcare system (Dinulus, 2020). This case report illustrates the complexities of managing ADRs in patients with a complicated treatment history, factoring in an evolving therapeutic landscape that may obfuscate main medical problems in at-risk populations. Moreover, this case stresses the need to study rarer side effect profiles of drugs used to treat these patients, mitigate risks, and optimize health outcomes.
Case:
We report a case of a 58-year-old female with a history of anxiety, depression, psychosis, lymphedema, recurrent cellulitis, and eczema experiencing a severe dermatological reaction. Psychiatry was consulted to assess medications addressing psychosis. Evaluation included medication history, admission labs, and consults by other specialties. Labs indicated leukocytosis, eosinophilia, elevated TSH, and extensive skin rash with lymphadenopathy were found on physical exam. A potential link between the patient's medication adjustments and the observed clinical complications was explored. The patient's presentation was consistent with a drug reaction with eosinophilia and systemic symptoms (DRESS Syndrome), determined to likely be a reaction to recently prescribed medication. She was transferred to the medicine-psychiatry unit (MPU) for psychiatric co-management as well as an improved environment. Furthermore, the MPU facilitated a collaborative, patient-centric approach. The patient had endorsed recent high-dose paliperidone use and rapid discontinuation, which represents a novel case of paliperidone-induced DRESS syndrome. A thorough review of patient history, interdisciplinary care, discontinued psychiatric medications, and treatment with corticosteroids and antihistamines led to symptom resolution.
Discussion:
The possibility of ADRs gives importance to cautious approaches in managing medication adjustments. An emphasis on patient histories in a dynamic pharmacotherapeutic environment is essential as well. Clinical research must align with contemporary risks, especially with polypharmacy as a major public health concern, highlighting the need for systematic modernization of protocols to effectively prevent and manage potential ADRs in populations with complicated comorbidities. Furthermore, this case highlights the need for research into areas like pharmacogenomics to refine current strategies (Russa, 2017).
Conclusion/Implications:
Antipsychotic medication has been associated with a variety of dermatologic manifestations, including DRESS (FDA, 2019). Effective management of ADRs in complex patients requires an enhanced, collaborative effort. This was facilitated by the utilization of a psychiatry consultation and management at the MPU. This demonstrates the efficacy of an interdisciplinary patient-centric approach, underscoring the importance of comprehensive patient reviews in enhancing safety and treatment outcomes.
References:
- Clinical Dermatology: Diagnosis & Management of Common Disorders, (7th ed.). Lange.
- Research, C. for D. E. and. (2019). FDA Drug Safety Communication: FDA warns about rare, severe skin reactions with mental health drug olanzapine (Zyprexa et al.). FDA. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-warns-about-rare-serious-skin-reactions-mental-health-drug
- La Russa R, Fineschi V, Di Sanzo M, Gatto V, Santurro A, Martini G, Scopetti M, Frati P. Personalized Medicine, and Adverse Drug Reactions: The Experience of An Italian Teaching Hospital. Curr Pharm Biotechnol. 2017;18(3):274-281. doi: 10.2174/1389201018666170207124835. PMID: 28176638.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Mental health disorders disproportionately affect marginalized groups and impact lower socioeconomic demographics in our communities. People of color, members of the LGBTQ+ community, and those in low-income areas face barriers like disproportionate social impact of disease and a lack of access to care and resources. How the patient in this case was managed and treated, despite exhibiting complexities in care, inconsistent follow-up and medication history, and difficulty with multiple providers, exemplifies a strong, replicable methodology applicable in many clinical settings. Furthermore, highlighting these concerns is critical to address major gaps in acute care for all disaffected populations.

