Systems-Based Practice, Leadership, and Administrative Psychiatry
(192) Integrating Advocacy for Older Adults with Systems-Based C-L Practice: Intervention Opportunities Through the Lens of a Complex Case

Angelique D. Woods, MD (she/her/hers)
Resident Psychiatrist
The Ohio State University Wexner Medical Center
Columbus, Ohio.jpg)
David Kasick, MD, DFAPA, FACLP
Professor of Clinical Psychiatry and Behavioral Health
The Ohio State University Wexner Medical Center
Columbus, Ohio
Presenting Author(s)
Co-Author(s)
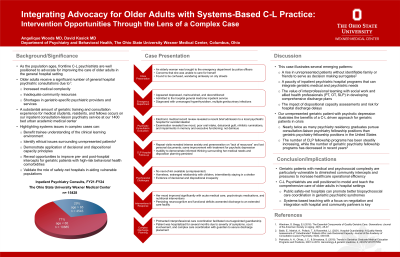
Background/Significance: Older adults receive a significant number of general hospital psychiatric consultations due to increased medical complexity, inadequate community resources, and shortages in geriatric-specific psychiatric provider and services (Warshaw 2016). As the population ages, it is imperative that frontline C-L psychiatrists advocate for opportunities to improve the care of older adults and highlight systems complexity for trainees in the clinical learning environment. We feature the case of an unrepresented geriatric patient with psychotic depression who presented to our safety-net hospital, illustrating the benefits of a C-L-driven approach for geriatric patients in crisis.
Case: An elderly woman was brought to the emergency department by police due to concerns that she was unable to care for herself after they found her wandering aimlessly on city streets. No next-of-kin was available. Following admission to the hospital, she was found to have unmanaged hyperthyroidism, multiple genitourinary infections, and appeared to be depressed, malnourished, and deconditioned. Psychiatric consultation revealed stable consciousness and awareness, but intense anxiety and perseveration on a “lack of resources” and lost personal documents. Electronic medical record review revealed a recent brief admission to a local psychiatric hospital for suicidal ideation complicated by homelessness, an estranged relationship with her children, with subsequent discharge to a shelter. Serial examinations revealed low mood, poor oral intake, feelings of guilt, nihilistic ruminations, and impairments in memory and executive functioning. She was unable to demonstrate informed thinking surrounding her medical care and disposition planning, prompting court-appointed guardianship and protracted interprofessional care coordination. Over several months, her mood improved significantly with acute medical care and psychotropic medication interventions for psychotic depression, although persisting neurocognitive and functional deficits warranted discharge to an extended care facility.
Discussion: Patients over age 65 comprise 29% of inpatient psychiatry consults at our 1400 bed urban academic medical center. This case illustrates several emerging clinical patterns: a rise in unrepresented patients without identifiable family or friends to serve as decision making surrogates (Babb, 2021), a paucity of inpatient psychiatric hospital programs that can integrate geriatric needs, and the value of interprofessional teaming with social work and allied health professionals to develop comprehensive discharge plans for patients with dispositional incapacity.
Conclusion/Implications: Geriatric patients with medical and psychosocial complexity are particularly vulnerable to diminished community intercepts and pressures to increase healthcare operational efficiency. As the number of CLP fellows has eclipsed geriatric psychiatry fellowship graduates in the United States, C-L psychiatrists are well positioned to model and teach the comprehensive care of older adults in hospital settings, particularly when public safety net hospitals are needed to coordinate the coexisting biopsychosocial elements in geriatric neurobehavioral syndromes.
References:
- Warshaw, G., Bragg, EJ. (2016). The Essential Components of Quality Geriatric Care. Generations: Journal of the American Society on Aging, 40(1), 28–37.
- Babb, E., Matrick, A., Pollack, T., & Rosenthal, L. J. (2021). Hospital Guardianship: A Quality Needs Assessment of "Unbefriended" Patients Who Lack Decisional Capacity. Journal of the Academy of Consultation-Liaison Psychiatry, 62(5), 538–545.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: As the population ages, it is imperative that frontline C-L psychiatrists recognize these risks facing geriatric patients, advocate for opportunities to improve the care of older adults, and demonstrate systems complexity for trainees in the clinical learning environment. A substantial amount of geriatric psychiatry training experience occurs on our inpatient CLP service, with excellent “teaching cases” featuring unique vulnerabilities surrounding decisional and dispositional incapacity. We encourage continued growth in this area of CL practice, particularly given the opportunity to model negotiation and system-based teaching skills with key hospital and community partners.

