Psycho-Oncology and Palliative Care
(118) Clozapine Continuation in a Patient Requiring Chemotherapy for Lymphoma
- JS
Jessica Schwartz, MD
Psychiatry Fellow
NYU Grossman School of Medicine
New York, New York - AM
Abby Mulkeen, MD
Attending Psychiatrist, Consultation-Liaison Service
NYU Langone Health
New York, New York - RC
Rachel Caravella, MD (she/her/hers)
Director, CL Psychiatry Service
NYU Langone Health
BRIARCLIFF MANOR, New York
Presenting Author(s)
Co-Author(s)
Background
Due to risk of agranulocytosis, questions remain about clozapine management in patients requiring myelosuppressive chemotherapy even when these regimens include granulocyte colony stimulating factors to support cell counts (Barreto 2015, Rausch 2020). Clozapine dose adjustment or discontinuation to avoid agranulocytosis risks psychotic decompensation, which may limit adherence with recommended cancer treatment, especially if other medical complications arise (Grainger 2019).
Case
A 56-year-old man with history of schizophrenia and over thirty years of symptom stability on clozapine 375mg by mouth daily was medically admitted for workup of new abdominal pain and distention, trouble breathing, and decreased urination. A large, intra-abdominal mass was discovered, and pathology confirmed a diagnosis of aggressive non-Hodgkin B-cell (Burkitt) lymphoma.
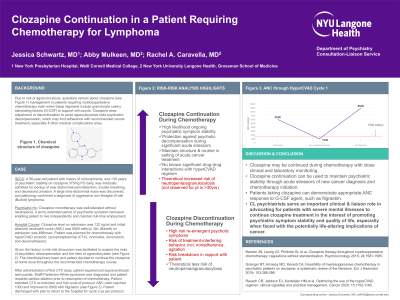
Further history confirmed that clozapine monotherapy was well-tolerated without neutropenia and that it led to extended period of psychiatric symptom remission, enabling patient to live independently and maintain full-time employment. Clozapine level on admission was 132 ng/mL and initial absolute neutrophil count (ANC) was 6000 cells/μl. Qtc at admission was 496msec with Bazett correction. Given the history, a risk-risk discussion was facilitated to explore the risks of psychiatric decompensation and the risks of agranulocytosis. The interdisciplinary team and patient decided to continue the clozapine at home dose through the recommended chemotherapy course.
Patient was planned for chemotherapy with hyperCVAD protocol, consisting of cyclophosphamide, vincristine, doxorubicin, and dexamethasone. After administration of first cyclophosphamide dose, patient experienced supraventricular tachycardia leading to diagnosis of Wolff-Parkinson-White syndrome. He underwent successful cardiac ablation and was able to resume chemotherapy as planned. Patient tolerated re-induction with cyclophosphamide and first cycle of protocol well. ANC reached a nadir of 1.0 during the cycle and improved to 8.9 with filgrastim. Patient was discharged with plan to return to the hospital for cycle 2 as per protocol.
Discussion
There is limited guidance regarding best practices for management of clozapine in patients requiring chemotherapy. For many patients, as in this case, clozapine is integral to psychiatric symptom remission. Such remission better enables patients to engage meaningfully with recommended medical care for serious conditions including cancer and to navigate complications. While this patient did experience a drop in ANC with hyperCVAD, an appropriate response to filgrastim was observed and treatment was able to proceed.
Conclusion
This case report suggests that clozapine may be continued during chemotherapy with close clinical and laboratory monitoring. Consultation-liaison Psychiatrists serve an important role in advocating for patients to continue clozapine treatment in the interest of ongoing psychiatric symptom stability and quality of life, especially when faced with the potentially life-altering implications of cancer.
References
Barreto JN, Leung JG, Philbrick KL et al. Clozapine therapy throughout myelosuppressive chemotherapy: regulations without standardization. Psychooncology 2015; 24:1581-1585.
Grainger BT, Arcasoy MO, Kenedi CA. Feasibility of myelosuppressive chemotherapy in psychiatric patients on clozapine: a systematic review of the literature. Eur J Haematol 2019; 103:266-286.
Rausch CR, Jabbour EJ, Kantarjian HM et al. Optimizing the use of the hyperCVAD regimen: clinical vignettes and practical management. Cancer 2020; 15:1152-1160.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: For this patient, comprehensive psychiatric treatment was offered during cancer treatment, including clozapine continuation despite inherent risks. For patients from marginalized and minoritized groups, access to high-quality psychiatric treatment, including clozapine, has been historically limited. There are well-documented patterns of inequitable care for patients with schizophrenia care based on race. Research shows that additional factors (eg. Benign Ethnic Neutropenia) may deter clinicians from prescribing clozapine even though no additional risk is posed. Our report demonstrates a framework for balancing multiple risk factors for clozapine, including benefits of psychiatric stability and quality of life for patients undergoing cancer treatment.

