Catatonia
(021) Charlson Comorbidity Index and Length of Hospitalization in Catatonia Subtypes

Edith Liliana Patarroyo Rodriguez
Resident Physician
Mayo Clinic
Rochester, Minnesota- LD
Laura Duque, MD
Neuropsychiatry Fellow
Massachusetts General Hospital
Boston, Massachusetts - BS
Balwinder Singh, MD, FAPA
Assistant Professor
Mayo Clinic
Rochester, Minnesota
Presenting Author(s)
Co-Author(s)
Background:
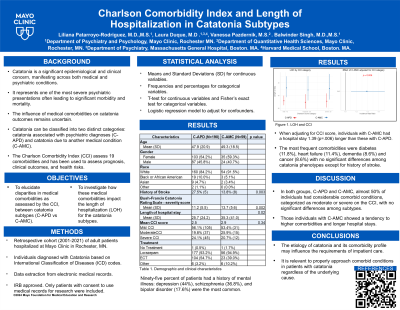
The influence of medical comorbidities on catatonia outcomes remains uncertain. We aimed to elucidate disparities in medical comorbidities, assessed by the Charlson Comorbidity Index (CCI), between catatonia subtypes: catatonia associated with psychiatric diagnoses (C-APD) versus catatonia due to another medical condition (C-AMC). Additionally, we investigated how these medical comorbidities impact the length of hospitalization (LOH) among catatonia subtypes.
Methods:
Our cohort included adults hospitalized at Mayo Clinic in Rochester, Minnesota, between May 1, 2001, and May 1, 2021, diagnosed with catatonia upon admission or during hospitalization (Ghafouri, 2024). The study was approved by the institutional review board and only patients who provided consent were included. Electronic medical records (EMR) were used to obtain clinical data and to confirm catatonia diagnosis. Data were managed using REDCap. Comorbidity profiles were assessed with the CCI, a prediction tool for long-term mortality based on comorbid conditions used to assess clinical outcomes and health risks (Charlson, 2022). Means and standard deviations for continuous variables, and frequencies and percentages for categorical variables, were used to summarize the data. Analysis of Variance or T-tests and Fisher's exact tests were employed for continuous and categorical variables, respectively.
Results:
Among the 250 hospitalized catatonic patients, 245 CCI scores were accessible. Mean age was 48.3 years, 86% of the patients were white, and 55.4% were female. Of these 187 (76.3%) were diagnosed with C-APD, while 58 (23.7%) were diagnosed with C-AMC. Bush-Francis Scale mean scores were 5.4 for screening items and 11.8 for severity. The mean CCI scores were similar between patients with C-APD (2.5) and C-AMC (2.9) (p=0.34). However, patients with C-AMC had higher prevalence of previous cerebrovascular accident (p=.003) compared to those with C-APD. No significant differences were observed in other medical comorbidities. LOH was longer for patients with C-AMC compared to those with C-APD (35.6 days vs 25.6 days, p=0.002). Mean LOH did not differ (p=0.96) based on the CCI categories (mild, moderate, severe). However, when analyzing the interaction between CCI categories and catatonia subtypes, significantly longer LOH was observed among C-AMC compared to C-APD in the mild CCI category only (38.8 vs 25.4 days, p=0.049). After adjusting for the baseline CCI category, C-AMC was associated with a 1.39 times longer LOH (95% CI 1.10 to 1.77) compared to those with C-APD (p=0.006).
Discussion:
Our data suggest that the etiology of catatonia and its comorbidity profile may influence the LOH, particularly in those with C-AMC
Conclusion:
While C-APD was predominant, C-AMC showed a tendency towards higher comorbidities, experienced longer LOH, and had higher prevalences of stroke. Insights provided by the CCI about patient’s health status could inform clinical outcomes, emphasizing the need for evaluation and treatment of comorbid conditions even in patients with a psychiatric etiology of catatonia. Further studies are warranted.
Charlson, Mary E., et al. "Charlson comorbidity index: a critical review of clinimetric properties." Psychotherapy and psychosomatics 91.1 (2022): 8-35.
Ghafouri, Mohammad, et al. "Identifying clinical predictors for considering brain FDG-PET imaging in patients with catatonia: A case-control study." Schizophrenia Research 267 (2024): 138-140.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: The three authors of this poster are international medical graduates. Two of the authors (Drs. Patarroyo-Rodriguez and Duque) represent the Latino women's minority.

