Psychopharmacology and Toxicology
(133) Case Report: An autoimmune encephalitis-like presentation of bupropion overdose in a 38-year-old woman
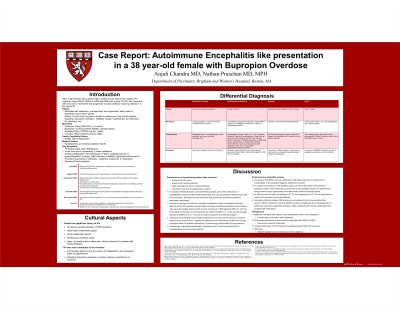

Anjali Chandra, MD (she/her/hers)
Resident Physician
Brigham and Women's Hospital
Cambridge, Massachusetts
Nathan Praschan, MD, MPH
Associate Psychiatrist
Brigham and Women's Hospital
Boston, Massachusetts
Presenting Author(s)
Co-Author(s)
Disclosure(s):
Anjali Chandra, MD: No financial relationships to disclose
Case: The patient was a 38-year-old woman with premenstrual dysphoria for which she had been prescribed bupropion. Two weeks prior to presentation, the patient complained of daily headaches leading to a sumatriptan prescription. One day prior, she developed sleep-wake disturbance and odd behaviors, followed by lethargy. The day of presentation, she was found unarousable and developed tonic-clonic movements. She was admitted to the neuro-ICU for status epilepticus and was loaded with multiple antiseizure medications. Between periods of stupor she was paranoid, hallucinating, agitated, and exhibited stereotypic movements of her arms without EEG correlate–although no other specific signs of catatonia. The initial workup was notable for hypertension, tachycardia, leukocytosis, and a prolonged QT. The differential diagnosis for her presentation included encephalitis, epilepsy and postictal psychosis, and overdose-related conditions (such as serotonin syndrome or hyperadrenergic/hyperdopaminergic states). Her APE2 was 4, and she received a lumbar puncture to rule out autoimmune as well as infectious encephalitis. Her agitation was managed with valproate, dexmedetomidine, and lorazepam given concerns for AE; and later, clonidine and quetiapine. She was treated with steroids, immunoglobulins, and acyclovir. Her mental status cleared within days. A bupropion/hydroxybupropion level taken from presentation returned consistent with acute overdose, which she could not recall. It became apparent she was experiencing intimate partner abuse, which may have played a role in the overdose–although concerns about AE precipitating the overdose remained until the serum and CSF panels returned negative. An involuntary hospitalization was considered, although rejected in favor of intensive outpatient treatment given her amnesia for the event, future orientation, and the need for a trauma-informed approach to long-term treatment planning.
Discussion: Bupropion overdose is well-described, at times characterized by psychosis, seizures, and agitation (1). This patient’s presentation, although ultimately ascribed to bupropion overdose, was concerning for acute encephalitis–a similarity with which consult psychiatrists should be familiar in the appropriate management of such patients. The bupropion/hydroxybupropion level was instrumental in proving an acute overdose in this patient (2). Holistic consideration of her psychosocial circumstances, including her history of trauma and need for ongoing psychiatric treatment in the context of ongoing abuse, led to a favorable outcome without involuntary hospitalization. This outcome should empower consult psychiatrists to consider lower levels of care, particularly in light of recent publications questioning the broad utility of involuntary hospitalizations (3, 4).
References
1. Alberter et al. Bupropion Toxicity. 2022. In: StatPearls. PMID: 35593803.
2. Costa et al. Pharmacokinetic and pharmacodynamic of bupropion. Drug Metab Rev. 2019. PMID: 31124380.
3. Deering et al. Ontological insecurity of inattentiveness: Conceptualizing how risk management practices impact on patient recovery when admitted to an acute psychiatric hospital. Int J Ment Health Nurs. 2024. PMID: 37882636.
4. Ross et al. Estimated Average Treatment Effect of Psychiatric Hospitalization in Patients With Suicidal Behaviors. JAMA Psychiatry. 2024. PMID: 37851457.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: This case presentation gives light to the psychosocial complexities underlying overdose. This patient identifies as an African American woman and experienced intimate partner violence (IPV). According to the Institute for Women's policy research, black women are more likely to experience IPV compared to white women, and three times as likely to die from the sequela. We feel this is an opportunity to share this patient's story and the good outcomes that resulted from considering her case holistically.
References
1. The Institute for Women's Policy Research. The Status of Black Women in the United States. Retrieved from https://iwpr.org/wp-content/uploads/2020/08/SOBW_ExecutiveSummary_Digital-2.pdf.

