Collaborative and Integrated Care
(052) Caring for the Adolescent Psychiatric Patient on an Adult Medical Unit

Robert Simons, MD
Resident Physician
Temple Univeristy Hospital
philadelphia, Pennsylvania
Danna Zevy, MD, MS
Resident Physician
Temple Health Chestnut Hill
Philadelphia, Pennsylvania.jpg)
Natalia Ortiz, MD
Chief Consultation and Liaison Psychiatry
Lewis Katz Temple School of Medicine
Philadelphia, Pennsylvania- JD
Jaclyn Dietzold, MD + CAP fellowship
Assistant Professor
Temple University
Philadelphia, Pennsylvania
Presenting Author(s)
Co-Author(s)
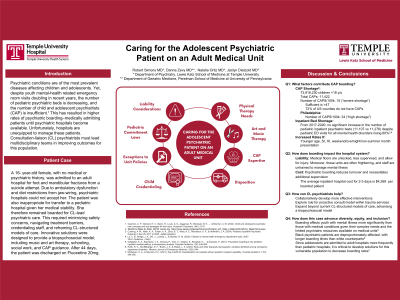
Background: Psychiatric conditions are of the most prevalent diseases affecting children and adolescents. Yet, despite youth mental-health related emergency room visits doubling in recent years, the number of pediatric psychiatric beds is decreasing, and the number of child and adolescent psychiatrists (CAP) is insufficient (Guerrero, 2022). This has resulted in higher rates of psychiatric boarding–medically admitting patients until psychiatric hospitals become available. Unfortunately, hospitals are unequipped to manage these patients. Consultation-liaison (CL) psychiatrists must lead multidisciplinary teams in improving outcomes for this population.
Case: A 16- year-old female, with no medical or psychiatric history, was admitted to an adult hospital for foot and mandibular fractures from a suicide attempt. Due to ambulatory dysfunction and diet restrictions from jaw-wiring, psychiatric hospitals could not accept her. The patient was also inappropriate for transfer to a pediatric hospital given her medical stability. She therefore remained boarded for CL-lead psychiatric care. This required minimizing safety concerns, navigating treatment barriers, credentialing staff, and reframing CL-structured models of care. Innovative solutions were designed to provide a biopsychosocial model, including music and art therapy, schooling, social work, and CAP guidance. After 44 days, the patient was discharged on Fluoxetine 20mg.
Discussion: Boarding affects youth with mental illness more significantly than those with medical conditions given their complex needs and the limited psychiatric resources available on medical units (Gallagher, 2017). Medical floors are unlocked, less supervised, and allow for injury. Moreover, these units are often frightening, and staff are untrained to manage mental illness. Psychiatric boarding is also costly, as it reduces turnover and necessitates additional supervision. Since adolescents are admitted to adult hospitals more frequently than pediatric hospitals, it is critical to develop solutions (Michelson, 2023). However, little literature exists on ways to achieve this. As boarding increases, CL psychiatrists must advance the current biopsychosocial model to help manage these individuals.
Conclusion: An adolescent patient was boarded for 44 days on an adult medical unit with injuries from a suicide attempt that prevented transfer to inpatient psychiatry. This required extending the biopsychosocial approach of inpatient psychiatry to a medical unit, where numerous barriers limited psychiatric care. As rates of youth boarding increase, CL psychiatrists must collaboratively intervene for this population. Expanding beyond current CL-structured models of care may also decrease transfer rates to inpatient psychiatry and, therefore, increase bed availability. This case highlights the need for creative solutions for boarded youth so that providers are better equipped to navigate their psychiatric care.
References:
Guerrero, A. P., Beresin, E. V., Balon, R., Louie, A. K., Aggarwal, R., Morreale, M. K., ... & Brenner, A. M. (2022). Child and adolescent psychiatry: New concepts and new strategies for the future. Academic Psychiatry, 46(1), 6-10.
Gallagher, K. A., Bujoreanu, I. S., Cheung, P., Choi, C., Golden, S., Brodziak, K., ... & Ibeziako, P. (2017). Psychiatric boarding in the pediatric inpatient medical setting: a retrospective analysis. Hospital Pediatrics, 7(8), 444-450.
Michelson, K. A., & Neuman, M. I. (2021). Age cutoffs for hospitalization at hospitals without pediatric inpatient capability. Hospital pediatrics, 11(3), 284-286.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: The number of child and adolescent psychiatrists and inpatient psychiatric beds does not meet patient needs, which has led to increasing rates of psychiatric boarding. Boarding affects youth with mental illness more significantly than those with medical conditions, as medical units are unequipped to manage their complex needs. Of this already marginalized group, black patients are disproportionately affected, with longer boarding times than white counterparts (Ruffo, The Western Journal of Emergency Medicine, 2022). Consultation-liaison psychiatrists must develop more effective interventions so that teams caring for this vulnerable population will be better equipped to navigate their psychiatric care more equitably.

