Delirium
(070) Missed Opportunities: Reactive vs. Proactive Consultation Rates for Delirium in a Medical Intensive Care Unit – Measuring Potential Impact of a Population-Based Multicomponent Model for Early Intervention to Optimize Brain Health

Kevin Lam, MD (he/him/his)
Psychiatry Resident
Rutgers: Robert Wood Johnson Medical School
Highland park, New Jersey
Elisabeth Dietrich, MD (she/her/hers)
Consultation-Liaison Psychiatry Fellow
Brigham and Women's Hospital
Henrico, Virginia
Michael Kusnet, BA
Medical Student (M4)
VCU School of Medicine
Richmond, Virginia- EN
Elyse Nguyen, BS
Medical Student
Virginia Commonwealth University
Richmond, Virginia 
Melissa Bui, MD
Associate Professor of Psychiatry
Virginia Commonwealth University
Richmond, Virginia
Presenting Author(s)
Co-Author(s)
1. Bienvenu, doi:10.1016/j.genhosppsych.2023.11.006 2. Bui, doi:10.1016/j.psym.2018.07.011 3. Bronson, doi:10.1016/j.jaclp.2021.12.008 4. Choi, doi:10.1016/j.jpsychires.2023.02.011 5. Inouye, doi:10.1016/S0140-6736(13)60688-1
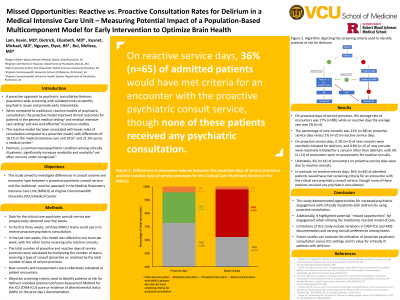
Background: A proactive approach to psychiatric consultation features population-wide screening with validated tools to identify psychiatric issues and provide early intervention. Previous studies demonstrated that when compared to traditional, reactive psychiatric consult models, the proactive model improved clinical outcomes for patients in the general medical setting1 and medical intensive care setting2, and was cost-effective.3 The reactive model has been associated with lower consult rates compared to a proactive model, with differences of 18.1% in the medical intensive care unit (ICU)2 and 21.3% across a medical center.1 Delirium, a common neuropsychiatric condition among critically ill patients, significantly increases morbidity and mortality4 yet often remains under-recognized.5 This study aimed to investigate differences in consult volume and encounter type between a proactive psychiatric consult service and the traditional, reactive approach in the Medical Respiratory Intensive Care Unit (MRICU) at Virginia Commonwealth University (VCU) Medical Center.
Methods: Data for the proactive psychiatric consult service was prospectively obtained over five weeks. In the first three weeks, all three MRICU teams could opt in to receive proactive consults. In the last two weeks, this model was offered to one team per week, with the other teams receiving only reactive consults. The total number of proactive and reactive days of service provision were calculated by multiplying the number of teams receiving a type of consult (proactive vs. reactive) by the total number of days of service provision. New consults and reassessments were collectively tabulated as patient encounters. Objective screening criteria used to identify patients at risk for delirium included positive Confusion Assessment Method for the ICU (CAM-ICU) score or evidence of altered mental status (AMS) on the prior day’s documentation.
Results: On proactive days of service provision, the average consult rate was 27% (n=88), while on reactive days the rate was 2% (n=4). The percentage of new consults was 12% (n=38) on proactive service days versus 1% (n=2) on reactive service days. Ultimately, 4% (n=14) of encounters on proactive service days were due to reactive consults. In contrast, on reactive service days, 36% (n=65) of admitted patients would have met criteria for an encounter with the proactive psychiatric consult service, though none of these patients received any psychiatric consultation. .
Discussion: Limitations of this study include variations in CAM-ICU and AMS documentation and varying consult preferences among teams. Future studies can evaluate the utilization of proactive psychiatric consultation across ICU settings and its value for critically ill patients with delirium.
Conclusion: This study demonstrated increased engagement with critically ill patients with delirium by using a proactive psychiatric consult model. Additionally, it highlighted potential “missed opportunities” for clinical care engagement when using a traditional consult model.
References:
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Arias et al. (2020, 2023) and Shiff et al. (2022) highlighted the influence of social determinants of health, such as neighborhood disadvantage, blue-collar occupation, and paternal education on delirium incidence and severity. Haddad, et al. (2020) identified racial and educational disparities in post-ICU cognitive outcomes. These findings underscore potential connections between socio-economic factors and outcomes, particularly in the context of delirium. Our findings suggest that proactive consults may lead to a reduction in missed encounters, enhancing the equity of healthcare delivery. Future goals will be to improve screening to ensure that all patients, regardless of background, have equitable access.

