Transplant Psychiatry and C-L Subspecialties
(216) Mind the Gap: Exploring the Mental Health Needs of Cystic Fibrosis Patients Who Undergo Lung Transplantation
- SW
Shannon Wright, RN(EC) NP-PHC, MSc., CPMHN(C)
Nurse Practitioner
Universtiy Health Network
Toronto, Ontario, Canada - SB
Sarah J. Beneteau, RN-EC, PHC-NP (she/her/hers)
Nurse Practitioner, Psychiatry
University Health Network, University of Toronto
Toronto, Ontario, Canada - LW
Lisa Wickerson, PhD
Affiliate Scientist
University Health Network
Toronto, Ontario, Canada - JS
Julie Statler, MSc, RD
Registered Dietitian
Toronto General Hospital
Toronto, Ontario, Canada - JW
June Wang, BScPhm
Clinical Pharmacist
Ajmera Transplant Program, University Health Network
Toronto, Ontario, Canada - CC
Cecilia B. Chaparro, MD, MsC
Lung transplant and Cystic Fibrosis Respirologist
Toronto Lung Transplant Program and St. Michael's Hospital
Toronto, Ontario, Canada 
Susan E. Abbey, MD, FRCPC, FACLP
Program Medical Director
Program Medical Director
Toronto, Ontario, Canada
Presenting Author(s)
Co-Author(s)
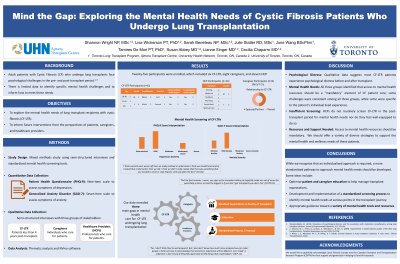
Background: Adult cystic fibrosis (CF) patients who undergo lung transplant experience an increase in psychological distress in the early post-transplant period (Chu et al., 2018; Rynar et al, 2018) . At present, there is limited data to inform what, if any, intervention would support patients, caregivers, and health care providers in meeting the mental health needs of CF lung transplant recipients (CF-LTR). The aim of this study is to explore the mental health needs of CF-LTR and to inform future patient-centred interventions that are relevant from a patient, caregiver and healthcare provider (HCP) perspective.
Methods: Mixed methods study using semi-structured interviews and standardized mental health screening tools.
Quantitative Data Collection: CF-LTR participants completed both the Patient Health Questionnaire nine item scale (PHQ-9) and the Generalized Anxiety Disorder seven item scale (GAD-7).
Qualitative Data Collection: Semi-structured interviews with 3 stakeholder groups (CF-LTR < 4 years post-transplant, their caregivers, and HCPs) to explore the lived experience of CF-LTR in the post-transplant period, identify if there are any unmet mental health needs, and explore how these needs could be better addressed.
Results: Twenty-five participants were enrolled, which included six CF-LTR, seven caregivers, and eleven HCP.
CF-LTR Participants (n=6):
Age | Gender | Race/Ethnicity | Type of Tx | Hx of MH Support | Current MH Support | ||||||
18-30 | 2 | M | 2 | White | 5 | First DLTx | 5 | Yes | 3 | Yes | 3 |
31-64 | 3 | ||||||||||
65+ | 1 | F | 4 | Métis | 1 | Second DLTx | 1 | No | 3 | No | 3 |
Caregiver Participants (n=8):
Gender | Relationship to CF-LTR | ||
M | 3 | Spouse/Partner | 4 |
F | 5 | Parent | 4 |
HCP Participants (n=11):
Gender | Discipline | |||
M | 2 | Nursing | 5 | |
Spiritual Care | 1 | |||
Medicine | 2 | |||
Nutrition | 1 | |||
Social Work | 1 | |||
F | 9 | Pharmacy | 1 | |
Thematic analysis is currently underway, through a collaborative and iterative process of reading/listening and coding.
Discussion: Preliminary results indicate the majority of CF-LTR experienced psychological distress in the early post-transplant period. CF-LTR and their caregivers identified that access to mental health resources should be a “mandatory” element of their care and needs to be embedded throughout their transplant journey. HCPs do not routinely screen CF-LTR in the post-transplant period for mental health needs nor do they feel well-equipped to do so. Final analysis of data will reveal future patient-centred interventions that are relevant from a patient and healthcare provider perspective.
Conclusions: This study addresses the current gap in the literature regarding the unique mental health needs of CF-LTR and the mental health care they receive. The data from this study will inform future patient-centered interventions that may support best practice guidelines in lung transplant programs and transplant mental health programs.
References:
Chu, M. C., Smith, P. J., Stonerock, G. L., & Blumenthal, J. A. (2018). Depressive symptoms, medication nonadherence, and clinical outcomes following lung transplantation. American Journal of Transplantation, 18 (Supplement 4), 984.
Rynar, L. Z., Merchant, M. S., & Dilling, D. F. (2018). Suicidal ideation in lung transplant recipients: A case series. Clinical Transplantation, 32(6).
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: This research explores the challenges experienced by individuals who are living with a chronic medical condition and the impact it has on their mental health. To ensure the viewpoints of this specific population were reflected in the research, patient partners with lived experience informed the development of the qualitative interview questions.

