Catatonia
(024) Mild Encephalitis with Reversible Splenial Lesion (MERS) and Catatonia without Comorbid Mental Illness

Nicolas D. Iadarola, MD MS
Resident
University of Maryland Medical Center/Sheppard Pratt
Baltimore, Maryland
ANIQUE K. Forrester, MD
Assistant Professor
University of Maryland School of Medicine
Baltimore, Maryland
Presenting Author(s)
Co-Author(s)
Background/Significance: Although catatonia is frequently associated with severe mental illness, a significant number of cases (approximately 20%) are found to be rooted in a somatic etiology, with over two-thirds of those cases associated with CNS-specific disease (Oldham, 2018). As such, consideration of non-psychiatric etiologies is important in the work-up of patients presenting with catatonic features. Here, we present an illustrative case of a patient with Mild Encephalitis with Reversible Splenial Lesion (MERS) referred for primary concern for catatonia.
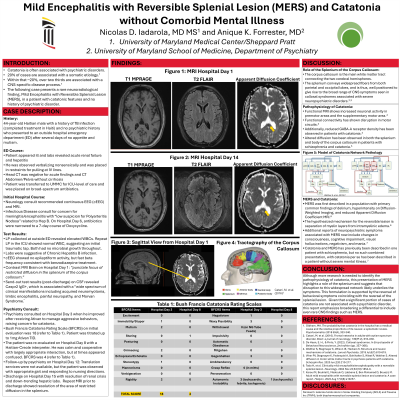
Case: “Mr. I” is a 44-year-old Haitian male with a medical history of treated tuberculosis and no prior psychiatric history who presented to an outside hospital after two days of altered mental status, poor appetite, and mutism associated with fever. The p</span>atient was transferred to the Univ of Maryland Medical Center after being found to be in multi-organ failure (acute renal failure and acute hepatitis). The p</span>sychiatry CL service was consulted after the patient received Ativan and his mental status improved. Initial work-up for etiology of organ failure and altered mentation, including LP and noncontrast CT of the head, were noncontributory. However, brain MRI with contrast revealed a punctate focus of restricted diffusion in the splenium of the corpus callosum. His initial Bush Francis Catatonia Rating Scale was 18. This constellation of symptoms; catatonia, changes in consciousness and cognition, and negativism-along with his neuroimaging results, suggested a diagnosis of MERS. His clinical course and mentation improved following an Ativan trial with a maximum total dose of Ativan 3mg over hospitalization. Prior to discharge on hospital day 14, repeat MRI Brain demonstrated resolution of the splenium lesion, which coincided with improvement in his symptoms. Discussion: Although catatonia now occupies an independent DSM-5 category, it remains commonly considered as a comorbid presentation with severe mental illness. MERS was first characterized by Tada and colleagues (2004), with many of that cohort presenting with delirium. Additional neuropsychiatric symptoms associated with MERS include changes in consciousness, cognitive impairment, visual hallucinations, negativism, and mania. Karoui and colleagues (2022) presented the first case of catatonia associated with MERS in a patient with schizophrenia. Our case serves to further delineate MERS and emphasize that non-psychiatric causes must be considered in the work up of patients presenting with symptoms of catatonia. Conclusion/Implications: MERS remains a rare finding, and presentations can vary. It is, therefore, crucial to carefully detail associated symptoms and to consider CNS etiologies. Additionally, neuropsychiatric presentations associated with MERS help to further elucidate the behavioral role of the splenium. References: Oldham, MA: The probability that catatonia in the hospital has a medical cause and the relative proportions of its causes: a systematic review. Psychosomatics 2018 59(4), 333-340. Tada H, et al. Clinically mild encephalitis/encephalopathy with a reversible splenial lesion. Neurology. 2004 Nov 23;63(10):1854-8. Karoui M, Bouhlel E, Maatouk O, Labbene E, Ben Mohamed D, Bouaziz M. Adult mild encephalitis with reversible splenial lesion and catatonia: A case report. Heliyon. 2022 Aug 17;8(8):e10257.
Presentation Eligibility: There has been no formal effort to write this case for publication. However, given the rarity of the presentation, we feel that it could be appropriate for publication as a case report in the future.
Diversity, Equity, and Inclusion: The case addresses multiple inequities, as our patient is a person of color, immigrant, and who faced the presumption of a primary psychiatric illness. Aspects of his course feature the challenge of bridging care across two countries of vastly different resources. Additionally, this case overall demonstrates that patients presenting with catatonia often are presumed to have primary psychiatric disorders, when a complete medical work up to rule out non-psychiatric causes is necessary.

