Collaborative and Integrated Care
(060) Let’s work together: Filling the gaps in care through a Psychiatry-Pediatric Collaborative Care Lecture Series
- AA
Arham Ahmad, MD
PGY-3 Resident
BronxCare Health Systems
New York, New York - BS
Bibiana Mary Susaimanickam, n/a
Director - Promoveo Psychiatry and Wellness
Bronxcare health Systems
Pompano beach, Florida - SB
Saif Bashir, MD
PGY-2 Psychiatry Resident
Psychiatry Residency Program BronxCare Health System
Fort Lee, New Jersey - CT
Chenique Texeira, MD
Resident
BronxCare
New York, New York 
Natasha Kasulis, MD
Resident
BronxCare Psychiatry
New York, New York
Presenting Author(s)
Co-Author(s)
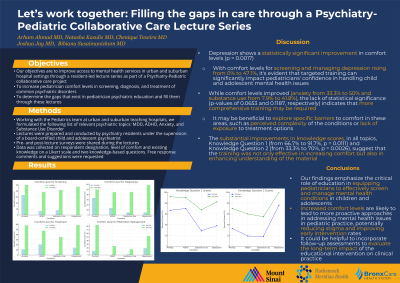
Objectives: Our institution developed a lecture series as the beginning of a continuing Pediatric collaborative care partnership. This series has thus far included lectures on Major Depressive Disorder (MDD), Attention Deficit/Hyperactivity Disorder (ADHD), Anxiety Disorders, and Substance Use Disorders (SUD). Using pre- and post-lecture surveys, our objectives were to determine what our pediatrician colleagues are looking for in their education on common psychiatric issues.We also looked at comfort levels regarding screening, diagnosis, and treatment before and after lectures were provided.
Methods: Coaching is provided through standardized lectures delivered by residents, curated by and under the supervision of board-certified child psychiatrists, covering common psychiatric illnesses and their management. Seven lectures have been delivered to our Pediatrics department covering 4 topics thus far: MDD, ADHD, Anxiety, and SUD. Each had a pre- and post-lecture survey shared via email and as a QR Code embedded within the presentation. We collected data on respondent type (Resident, Attending, Medical Student, etc.), level of comfort with aspects of delivering care, level of existing knowledge on the subject rated on a Likert scale, and 2 multiple choice questions based on the information presented. Finally, both surveys included free response sections for attendees to express their further interests in the topic.
Results: So far we have conducted 7 lectures on the topics of MDD, ADHD, Anxiety, and SUD between 2023 and 2024. The following results were gathered from our efficacy assessment tool. It consisted mostly of pediatric residents and attendings. Statistical analysis with chi-square tests were done for each category of questions in survey-screening, diagnosing and treatment. Based on the chi-squared tests, there are significant differences (P < 0.05) in improvement of comfort levels for SUD, ADHD in all categories, and for depression and anxiety treatment between the pre and post 2023/2024 responses. There were no significant changes noted for anxiety and depression screening. The percentage of correct responses on the knowledge-based questions increased by an average of 26% from before to after lectures. Finally, free response comments mostly consisted of the terms "treatment" and "medication management."
Conclusions: In this ongoing series we have learned that our pediatricians want more education on the treatment of pediatric psychiatric issues and are eager to participate in breaking down barriers to accessing timely psychiatric care. Through our model, our findings show an increased comfort level in our audiences regarding screening, diagnosing, and treating psychiatric disorders. The results also show some comfort level in screening for anxiety and depression as most medical records systems have screening tools embedded in them. Our pediatrician colleagues note the struggle with treating and getting referrals for these patients that have been identified with issues. We hope this project will result in higher rates of initiating psychiatric treatment by pediatricians and reduce wait times experienced in the context of psychiatrist shortages. As departments navigate the barriers of establishing full-fledged collaborative care models, starting these lectures for pediatric and family medicine clinicians will help patients in dire need for psychiatric care early on in primary care setting.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Bronx serves a diverse community. Children here face multiple social determinants of health, including decreased access to mental health services, exposure to adverse childhood experiences, poverty, chronic exposure to racism and community trauma. They also navigate challenges of stigma against mental health, which can perpetuate the already limited access to mental health services and long waitlists.PCP's are generally more trusted, accessible, & the first-line of contact.We hope to reduce barriers to accessing care by improving knowledge and comfort levels in managing common psychiatric issues. Education of residents will also help dispel common misunderstandings and disparities in delivery of psychiatric care

