Neurocognitive Disorders and Neuropsychiatry
(099) Sinonasal Squamous Cell Carcinoma with Intracranial Extension Presenting as Rapidly Progressive Dementia with Frontal Lobe Dysfunction

Rachel Brown, MD (she/her/hers)
PGY-2 Resident Physician
UPMC Western Psychiatric Hospital
Pittsburgh, Pennsylvania
Rachel Brown, MD (she/her/hers)
PGY-2 Resident Physician
UPMC Western Psychiatric Hospital
Pittsburgh, Pennsylvania.jpg)
Priyanka Amin, MD
Assistant Professor
UPMC Western Psychiatric Hospital
Pittsburgh, Pennsylvania.jpg)
Priyanka Amin, MD
Assistant Professor
UPMC Western Psychiatric Hospital
Pittsburgh, Pennsylvania
Jonathan Punzi, MD (he/him/his)
Assistant Professor of Psychiatry
UPMC Western Psychiatric Hospital
Pittsburgh, Pennsylvania
Jonathan Punzi, MD (he/him/his)
Assistant Professor of Psychiatry
UPMC Western Psychiatric Hospital
Pittsburgh, Pennsylvania
Presenting Author(s)
Co-Author(s)
Background/Significance:
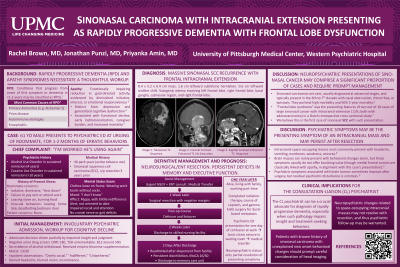
This case outlines the unusual presentation of a patient who presented to a psychiatric emergency department with features consistent with rapidly progressive dementia with frontal lobe dysfunction. To our knowledge this is the first case described in literature of sinonasal squamous cell carcinoma (SCC) presenting as frontal lobe dysfunction with persistent neuropsychiatric symptoms despite tumor resection, highlighting the psychiatrist's role in distinguishing structural frontal lobe pathology from primary mood, psychotic, and substance use disorders.
Case:
Mr. B is a male in his 60s with alcohol and cocaine use disorders in sustained remission and history of sinonasal SCC (s/p 2020 resection) who was brought to a psychiatric emergency department by his roommate due to one month of progressive functional decline.
He had stopped attending work, failed to pay rent, lost twenty pounds, and burned food on the stove, ignoring his smoke alarm. Mental status exam demonstrated blithely unconcerned/apathetic affect with impaired concentration and short-term memory. Screening neurologic exam was unrevealing beyond report of anosmia. Urine drug screen was negative.
He was involuntarily committed due to inability to care for himself. Initial differential included rapidly progressive dementia (e.g. due to recurrent carcinoma with brain metastases or paraneoplastic process), frontotemporal dementia, substance-induced neurocognitive disorder, and mood disorder.
Brain MRI revealed a 5x6x8cm sinonasal tumor with frontal intracranial extension and significant vasogenic edema. His presenting symptoms were attributed to frontal lobe edema and mass effect. Surgical resection was completed after transfer to the medical hospital. Residual neuropsychiatric symptoms persisted following resection (e.g. jocularity, disinhibition, memory impairment).
Discussion:
To our knowledge, this is the first case study of frontal lobe dysfunction as the primary presenting complaint of sinonasal SCC. Mr. B demonstrated typical demographic characteristics of sinonasal carcinoma—a white male around 60 with tobacco use history—though he lacked common presenting symptoms (nasal obstruction, epistaxis, and rhinorrhea).
Intracranial extension is a rare SCC complication with high morbidity. One Dutch cross-sectional study of large sinonasal tumors with intracranial extension showed that most presented with nasal obstruction or rhinorrhea, though 11% also experienced frontal lobe syndrome.1
While case studies show psychiatric symptoms often resolve following resection,2 Mr. B had residual symptoms post-resection.
Conclusion/Implications:
Our case underscores the role of the emergency/consultation-liaison psychiatrist in initiating workup of new onset frontal lobe dysfunction, as such pathology may interfere with patient self-advocacy and treatment-seeking behaviors. Although urgent imaging is rarely indicated in new onset frontal lobe pathology with a normal neurologic exam, timely head imaging may be crucial in patients with history of head and neck cancer. Furthermore, the consultation-liaison psychiatrist should recognize that neuropsychiatric symptoms may persist for months after tumor resection.
References:
1. Keizer, M. E., Hovinga, K. E., Lacko, M., Eekers, D. B., Baijens, L. W., Kremer, B., & Temel, Y. (2023). Clinical Outcome in Patients with Large Sinonasal Tumors with Intracranial Extension. Journal of Neurological Surgery Part B: Skull Base.
2. Madhusoodanan, S., Ting, M. B., Farah, T., & Ugur, U. (2015). Psychiatric aspects of brain tumors: a review. World journal of psychiatry, 5(3), 273.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Our submission focuses on timely recognition and workup for structural frontal lobe pathology/rapidly progressive dementia, ultimately identified as recurrent sinonasal carcinoma. ENT literature demonstrates a racial disparity in survival between black, Hispanic, and white patients for sinonasal carcinoma, largely mediated by stage and whether patients receive standard of care. Likewise, there are racial disparities present regarding workup and time to diagnosis for dementia more broadly. Our case offers the opportunity to review our role as psychiatrists in understanding and combating the racial disparities for workup of dementia and advocacy for patients when structural causes of dementia are identified.

