Psychopharmacology and Toxicology
(148) Review of Clozapine-Related Intestinal Perforation

Bekir Nihat Dogrul, MD
Psychiatry Resident
University of Rochester Medical Center
Rochester, New York- KR
Kyle Rodenbach, MD
Clinical Assistant Professor
University of Rochester Medical Center
Rochester, New York
Presenting Author(s)
Co-Author(s)
Background
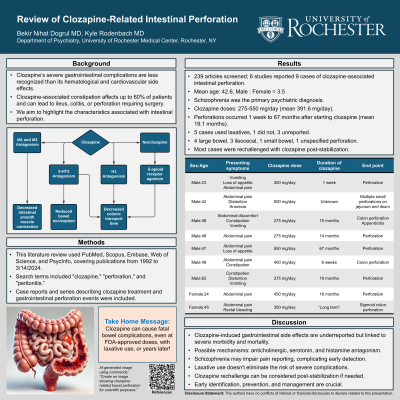
Clozapine, commonly prescribed for treatment-refractory schizophrenia, causes challenging side effects. While hematological and cardiovascular side effects are well established, severe gastrointestinal complications have received less attention (Díaz-Caneja, 2010). Observed in up to 60% of patients, clozapine-associated constipation can lead to complications such as ileus, colitis, or perforation necessitating surgical intervention (Ikai, 2013). This review aims to highlight the characteristics associated with intestinal perforation.
Methods
A literature search of English articles was conducted within PubMed, Scopus, Embase, Web of Science, PsycInfo, published between 1992 to 3/14/2024. Search terms included “clozapine”, “perforation” and “peritonitis”. Case reports and series which described clozapine treatment and any perforation event in the gastrointestinal system were included. We did not include cases of ileus or colitis without perforation, or case reports which omitted the medical characteristics of the cases. Sex, age, psychiatric diagnosis, clozapine dose and duration, laxative use, and perforation location were extracted.
Results
A total of 239 articles were screened, and 6 studies were included. Nine cases of clozapine use and intestinal perforation were reported. The mean age was 42.6 years with male predominance (M:F = 3.5). Schizophrenia was the primary psychiatric diagnosis in these cases. Clozapine doses ranged from 275 to 550 mg/day, with a mean dose of 391.6 mg/day at the time of perforation. Perforations occurred within a range of 1 week to 67 months after initiating clozapine, with an average duration of 19.1 months when excluding unreported data. Five cases were using laxatives with clozapine; one case was not prescribed laxatives, and the rest had unreported laxative use. Among nine cases, four large bowel, three ileocecal, one small bowel, and one unspecified bowel perforation were reported. Three out of nine cases were also diagnosed as appendicitis, and one had Meckel’s diverticulitis. Most cases were rechallenged with clozapine after stabilization, while a few switched to other atypical antipsychotics.
Discussion
While clozapine-induced gastrointestinal side effects have received less attention in the literature, our review suggests an association with severe morbidity and mortality. Possible mechanisms for clozapine-induced constipation might involve anticholinergic effects, serotonin, and histamine antagonism (Xu, 2021). Additionally, patients with schizophrenia may have difficulty reporting pain in ways physicians understand and this could make early detection of gastrointestinal complications more challenging (Carrasco-Picazo, 2023). Early identification, prevention, and management of clozapine-induced gastrointestinal side effects are crucial.
References
Díaz-Caneja CM, González-Molinier M, Galindo JC, Iñiguez MM. Severe Bowel Ischemia Due to Clozapine With Complete Remission After Withdrawal. J Clin Psychopharmacol. 2010;30(4):463-465.
Ikai S, Suzuki T, Uchida H, Mimura M, Fujii Y. Reintroduction of Clozapine After Perforation of the Large Intestine—A Case Report and Review of the Literature. Ann Pharmacother. 2013;47(7-8):e31-e31.
Xu Y, Amdanee N, Zhang X. Antipsychotic-Induced Constipation: A Review of the Pathogenesis, Clinical Diagnosis, and Treatment. CNS Drugs. 2021;35(12):1265-1274.
Carrasco-Picazo JP, González-Teruel A, Gálvez-Llompart AM, Carbonell-Asins JA, Hernández-Viadel M. Pain sensitivity in patients with schizophrenia: a systematic review and meta-analysis. Actas Esp Psiquiatr. 2023;51(1):29-40.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: In medical literature, ongoing debates persist regarding pain perception in patients with schizophrenia. In these patients, flat affect could obscure the expression of pain, posing a significant challenge in diagnosing severe gastrointestinal complications. If clinicians focus solely on psychiatric presentation and ignore questioning possible gastrointestinal side effects, it could lead to significant morbidity and mortality.

