Obesity, Nutrition, and Eating Disorders
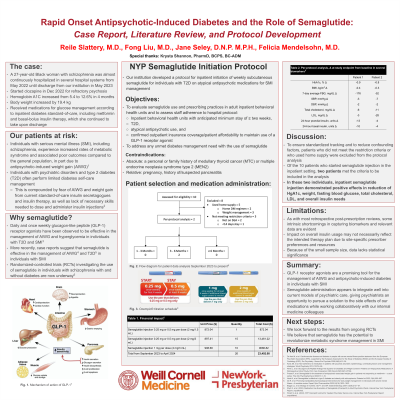
(114) Rapid Onset Antipsychotic-Induced Diabetes and the Role of Semaglutide: Case Report, Literature Review, and Protocol Development

Reile M. Slattery, MD (she/her/hers)
CL Psychiatry Fellow
New York University Langone Health
New York, New York- FL
Fong Liu, MD
Assistant Professor/ Attending Psychiatrist
Weill Cornell Medicine
New Rochelle, New York 
Jane J. Seley, DNP MPH FADCES
Assistant Professor of Medicine
Weill Cornell Medicine
New York, New York
Felicia A. Mendelsohn Curanaj, MD
Director, Inpatient Glycemic Management Program
Weill Cornell Medicine
Bayville, New York
Presenting Author(s)
Co-Author(s)
Background: Semaglutide has been demonstrated to facilitate achieving glycemic goals and reducing risk of major adverse cardiovascular events in individuals with type 2 diabetes (T2D). Individuals with serious mental illness (SMI) experience increased rates of metabolic syndrome and associated poor outcomes compared to the general population, in part due to antipsychotic-induced weight gain (AIWG). Here we report a case of rapid onset AIWG, diabetes, and hyperlipidemia, prompting our team to review the literature and develop a guideline for initiation and administration of semaglutide in select psychiatric inpatients.
Case: A 27-year-old Black woman with schizophrenia was almost continuously hospitalized from May 2022 until discharge in May 2023. She started taking clozapine in December 2022 for refractory psychosis. Four months later, she had gained 19.4 kg, and her hemoglobin A1C had increased from 5.4 to 12.6%. Her LDL increased from 114 to 143 mg/dL, and her serum triglycerides increased from 94 to 373 mg/dL. The individual received medications for glucose management according to the standard-of-care, including metformin and basal-bolus insulin therapy, which were continued upon discharge.
Discussion: Daily and once weekly glucagon-like peptide (GLP-1) receptor agonists have been observed to be effective in management of AIWG and hyperglycemia in individuals with T2D and SMI (Perlis, 2020). Case reports suggest that semaglutide specifically as a weekly injection is effective in the management of AIWG (Prasad, 2023) and T2D (Noda, 2022) in individuals with SMI. A narrative review revealed that clinical trials including randomized-controlled trials (RCTs) investigating the use of semaglutide in individuals with schizophrenia with and without diabetes are underway (De, 2023). Our institution has since developed a protocol for inpatient initiation of weekly subcutaneous semaglutide for individuals with T2D on atypical antipsychotic medications for SMI management (Parish, 2024). Several individuals are currently being monitored on the protocol, data pending.
Conclusion: GLP-1 receptor agonists are a promising tool for management of AIWG and antipsychotic-induced diabetes in individuals with SMI. Semaglutide administration integrates well into current models of psychiatric care, giving psychiatrists an opportunity to pursue a solution to the side effects of our medications while working collaboratively with our medicine colleagues. As access to our institution’s semaglutide protocol is limited to a small population, we look forward to results from ongoing RCTs. Semaglutide has the potential to revolutionize metabolic syndrome management in SMI.
References:
1) Perlis L, et al: Glucagon-Like Peptide Analogs Are Superior for Diabetes and Weight Control in Patients on Antipsychotic Medications: A Retrospective Cohort Study. Prim Care Companion CNS Disord 2020;22(1):27304.
2) Prasad F, et al: Semaglutide for the treatment of antipsychotic-associated weight gain in patients not responding to metformin – a case series. Ther Adv Psychopharmacol 2023;13:1–10.
3) Noda K, et al: Semaglutide is effective in type 2 diabetes and obesity with schizophrenia. Diabetol Int 2022;13(4):693–697.
4) De R, et al: Promising translatable pharmacological interventions for body weight management in individuals with severe mental illness—A narrative review. Expert Opin Pharmacother 2023; 24(16):1823–1832.
5) Parish S, et al. (2024). NYP Ozempic® Protocol. Internal New York-Presbyterian Report: unpublished.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Our case report centers an intersectional identity that is vulnerable and marginalized: a young Black woman with serious mental illness. The standard-of-care treatment of her refractory psychosis resulted in metabolic complications that jeopardized her health and lifespan. With the literature in mind, we propose an innovative semaglutide administration protocol to improve outcomes for psychiatric patients who systematically receive under-prioritized medical care in our current systems. Our author group is composed of a psychiatry resident going into consult-liaison fellowship, a chronic psychotic disorders unit chief, and two diabetes experts (nursing and internal medicine backgrounds), representing diversity of thought, education, and culture.

