Obesity, Nutrition, and Eating Disorders
(111) Palliative Care in Severe-Enduring Anorexia Nervosa: Giving up or Giving in?
- EK
Elizabeth M. Klein, MD (she/her/hers)
Resident Physician
University of Virginia Medical Center
Charlottesville, Virginia - AS
Anne Louise Stewart, MD
Assistant Professor
Univeristy of Virginia
Charlottesville, Virginia
Presenting Author(s)
Co-Author(s)
Background:
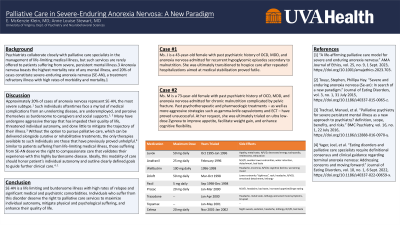
Psychiatrists collaborate closely with palliative care specialists in the management of life-limiting medical illness, but such services are rarely offered to patients suffering from severe, persistent mental illness.3 Anorexia nervosa boasts the highest mortality rate of any mental illness, and 20% of cases constitute severe-enduring anorexia nervosa (SE-AN), a treatment refractory illness with high rates of morbidity and mortality.1
Cases:
1. Ms. J is a 43-year-old female with past psychiatric history of OCD, MDD, and anorexia nervosa admitted for recurrent hypoglycemic episodes secondary to malnutrition. She was ultimately transitioned to hospice care after repeated hospitalizations aimed at medical stabilization proved futile.
2. Ms. M is a 73-year-old female with past psychiatric history of OCD, MDD, and anorexia nervosa admitted for chronic malnutrition complicated by pelvic fracture. Past psychotherapeutic and pharmacologic treatments – as well as more aggressive strategies such as gamma-knife capsulotomy and ECT – have proved unsuccessful. At her request, she was ultimately trialed on low-dose Zyprexa to improve appetite, facilitate weight gain, and enhance cognitive flexibility.
Discussion:
Approximately 20% of cases of anorexia nervosa represent SE-AN, the most severe subtype.1 Such individuals oftentimes face a myriad of medical complications from an unrelenting disease, are underemployed, and perceive themselves as burdensome.1,2 Many have undergone aggressive therapy that has impeded their quality of life, threatened individual autonomy, and done little to mitigate the trajectory of their illness.3 Without the option to pursue palliative care, which can be delivered alongside curative or rehabilitative treatments, the only therapies available to such individuals are those that have previously proved unhelpful.4 Similar to patients suffering from life-limiting medical illness, those suffering from SE-AN deserve the right to compassionate care that validates their experience with this highly burdensome disease. Ideally, this modality of care should honor patient’s lived experiences, maximize individual autonomy, and outline clearly defined goals to guide further clinical care.4, 1
Conclusion:
SE-AN is a highly lethal and burdensome illness with high rates of relapse and significant medical and psychiatric comorbidities. Individuals who suffer from this disorder deserve the right to palliative care services in order to maximize individual autonomy, mitigate physical and psychological suffering, and enhance their quality of life.
References
[1] “A life-affirming palliative care model for severe and enduring anorexia nervosa.” AMA Journal of Ethics, vol. 25, no. 9, 1 Sept. 2023, https://doi.org/10.1001/amajethics.2023.703.
[2] Touyz, Stephen, Phillipa Hay. “Severe and enduring anorexia nervosa (Se-an): In search of a new paradigm.” Journal of Eating Disorders, vol. 3, no. 1, 31 July 2015, https://doi.org/10.1186/s40337-015-0065-z.
[3] Trachsel, Manuel, et al. “Palliative psychiatry for severe persistent mental illness as a new approach to psychiatry? definition, scope, benefits, and risks.” BMC Psychiatry, vol. 16, no. 1, 22 July 2016, https://doi.org/10.1186/s12888-016-0970-y.
[4] Yager, Joel, et al. “Eating disorders and palliative care specialists require definitional consensus and clinical guidance regarding terminal anorexia nervosa: Addressing concerns and moving forward.” Journal of Eating Disorders, vol. 10, no. 1, 6 Sept. 2022, https://doi.org/10.1186/s40337-022-00659-x.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Psychiatrists collaborate with palliative care specialists to offer palliative care services to patients suffering from a wide array of medical illnesses, but rarely extend such services to patients of their own. Without the option to pursue palliative care, the only treatment options that patients with treatment refractory mental illness are left with are those that have previously proved unhelpful – and in some cases harmful. Patients with severe, persistent mental illness deserve the right to compassionate care that is readily offered to patients suffering from life limiting medical illnesses.

