Collaborative and Integrated Care
(062) Navigating Challenging Family Dynamics in the Acute Management of Anorexia Nervosa: A Multidisciplinary Approach
.jpeg.jpg)
Yi Ling Wang, MD (she/her/hers)
PGY-2 Resident
Zucker Hillside Hospital, Northwell Health
Glen Oaks, New York- MV
Maria Vasconez Narvaez, n/a
PGY-2 Resident
Zucker Hillside Hospital, Northwell Health
Manhasset, New York - SS
Shiana Sekhri, M.B.B.S
Consultation-Liaison Psychiatry Fellow
LIJ/Northwell Health
Jericho, New York - HS
Humaira Shoaib, MD
Consultation Liaison Psychiatrist
Long Island Jewish Medical Center, Northwell Health
New Hyde Park, New York 
Samuel Greenstein, MD
Consultation-Liaison Psychiatry Fellowship Director
Northwell
New Hyde Park, New York
Presenting Author(s)
Co-Author(s)
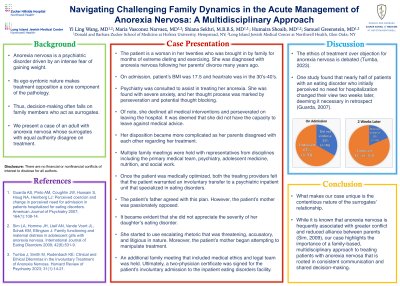
Background/Significance: Anorexia nervosa (AN) is a psychiatric disorder driven by an intense fear of gaining weight. Its egosyntonic nature makes treatment opposition a core component of the pathology. Thus, decision-making often falls on family members who act as surrogates. We present a case of an adult with AN whose surrogates with equal authority disagree on treatment.
Case: The patient is a female in her twenties who was brought in by her grandmother for months of extreme dieting and exercising. It was noted that she was diagnosed with AN following her parents’ divorce many years ago.
Psychiatry was consulted to assist in treating her anorexia. She was found to have severe anxiety, and her thought process was marked by perseveration and potential thought blocking. Of note, she declined all medical interventions and perseverated on leaving the hospital. It was deemed that she did not have the capacity to leave against medical advice. Her disposition became more complicated as her parents disagreed with each other regarding her treatment. Multiple family meetings were held with representatives from disciplines including the primary medical team, psychiatry, adolescent medicine, nutrition, and social work. Once the patient was medically optimized, both the treating providers felt that the patient warranted an involuntary transfer to a psychiatric inpatient unit that specialized in eating disorders. The patient’s father agreed with this plan. However, the patient’s mother was passionately opposed. It became evident that she did not appreciate the severity of her daughter’s eating disorder. She started to use escalating rhetoric that was threatening, accusatory, and litigious in nature. Moreover, the patient’s mother started to manipulate treatment; for instance, she attempted to remove the patient’s nasogastric tube. An additional family meeting that included medical ethics and legal team was held. Ultimately, a two-physician certificate was signed for the patient’s involuntary admission to the inpatient eating disorders facility.
Discussion: The ethics of treatment over objection for AN is debated (Tumba, 2023). One study found that nearly half of AN patients who initially perceived no need for hospitalization changed their view two weeks later, deeming it necessary in retrospect (Guarda, 2007). What makes our case unique is the contentious nature of the surrogates’ relationship. While it is known that AN is frequently associated with greater conflict and reduced alliance between parents (Sim, 2009), our case highlights the importance of a family-based, multidisciplinary approach to treating patients with AN that is rooted in consistent communication and shared decision-making.
References:
Guarda AS, Pinto AM, Coughlin JW, Hussain S, Haug NA, Heinberg LJ: Perceived coercion and change in perceived need for admission in patients hospitalized for eating disorders. American Journal of Psychiatry 2007; 164(1):108-14.
Sim LA, Homme JH, Lteif AN, Vande Voort JL, Schak KM, Ellingson J: Family functioning and maternal distress in adolescent girls with anorexia nervosa. International Journal of Eating Disorders 2009; 42(6):531-9.
Tumba J, Smith M, Rodenbach KE: Clinical and Ethical Dilemmas in the Involuntary Treatment of Anorexia Nervosa. Harvard Review of Psychiatry 2023; 31(1):14-21.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: The topic presented addresses equity in that anorexia nervosa predominantly affects adolescent or young adult women, a demographic that is traditionally underrepresented within the medical literature. Specifically, our abstract promotes the holistic assessment of individuals and their unique family dynamics in treatment planning. Furthermore, the authorship on this abstract is both racially/ethnically diverse and professionally inclusive, with representation from Asian-American, Hispanic/Latino, and South Asian backgrounds, as well as various levels of training. This abstract was the product of a collaborative effort by a team that included a PGY-1, PGY-2, CL fellow, CL attending, and CL fellowship director.

