Psychopharmacology and Toxicology
(140) Gestational Diabetes and Olanzapine: A Silent Time Bomb?

Elizabeth Clayton, MD (she/her/hers)
Resident
Albert Einstein-Montefiore Medical Center
NY, New York
Shilpa Lad, MD
Assistant Professor of Psychiatry, Albert Einstein College of Medicine
Montefiore Moses Hospital
Bronx, New York
Presenting Author(s)
Co-Author(s)
He Y, Fang W, Li Z, Sun L, Zhou Y, Wu C, Sun W, Wang C. Analysis of the clinical characteristics of olanzapine-induced acute pancreatitis. Ther Adv Psychopharmacol. 2022 Apr 29;12:20451253221079971. Ragucci KR, Wells BJ. Olanzapine-induced diabetic ketoacidosis. Ann Pharmacother. 2001 Dec;35(12):1556-8. Pace R, Brazeau AS, Meltzer S, et al. Conjoint Associations of Gestational Diabetes and Hypertension With Diabetes, Hypertension, and Cardiovascular Disease in Parents: A Retrospective Cohort Study. Am J Epidemiol 2017; 186:11
Background: Olanzapine, often used as a mood stabilizer, has been implicated in acute, new-onset diabetic ketoacidosis (DKA) without history of diabetes (DM), and acute pancreatitis (AP) without symptoms. Discontinuation of olanzapine typically leads to the normalization of laboratory values (1,2). Could starting this medication pose significant risk to patients with Gestational Diabetes?
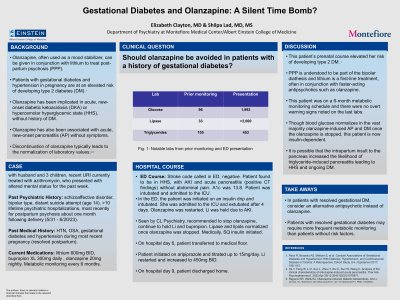
Case: 45-year-old African American female domiciled with husband and 3 children, PMH of HTN, OSA, gestational diabetes and hypertension during most recent pregnancy (resolved postpartum), PPH of schizoaffective disorder, bipolar type, distant suicide attempt (age 14), >10 lifetime admissions, last hospitalized for postpartum psychosis about one month following delivery (5/31 - 6/20/23), and was discharged on lithium 600mg BID, bupropion XL 300mg daily and olanzapine 20mg nightly. She was maintained on this regimen with metabolic monitoring every six months, which was unremarkable. On 3/9/24, she presented to the ED for altered mental status and was found to be in a severe hyperosmolar hyperglycemic state (HHS) with AKI and new-onset pancreatitis (lipase >2000, triglycerides 453; positive CT findings) without preceding abdominal pain. She had started a course of azithromycin in the week prior but otherwise had not changed her medications. She was admitted to the ICU, intubated and an insulin drip was initiated; all psychotropics were held. The patient’s condition improved and her lipase and lipids normalized once olanzapine was stopped. Care was downgraded to a medical floor, where she was started on aripiprazole and restarted on lithium, at a lower dose. She was able to be discharged home on this psychotropic regimen and with insulin.
Discussion: Patients with gestational diabetes and hypertension in pregnancy are at an elevated risk of developing type 2 DM (3). Postpartum psychosis is understood to be part of the bipolar diathesis and lithium is a first-line treatment, often in conjunction with faster-acting antipsychotics such as olanzapine. Though blood glucose normalizes in the vast majority olanzapine-induced AP and DM once the olanzapine is stopped, this patient is now insulin-dependent. It is possible that the intrapartum insult to the pancreas increased the likelihood of triglyceride-induced pancreatitis leading to HHS and ongoing DM.
Conclusion: For patients with resolved gestational diabetes, exploring alternative antipsychotics or implementing frequent metabolic screening is warranted in order to avoid HHS.
References:
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: This patient was an African American woman who was relatively recently postpartum, was being treated for schizoaffective disorder and presented with a medical emergency. Literature suggests that people of color, especially African Americans, are more likely to experience adverse events in the peripartum period. Treatment of postpartum psychosis may include olanzapine given that it has a faster onset as compared to lithium. This case indicates that gestational diabetes may put women at a higher risk for olanzapine-induced acute pancreatitis and dangerously high hyperglycemia. It highlights the importance of increased metabolic monitoring or using a different mood stabilizer in susceptible patients.

