Neurocognitive Disorders and Neuropsychiatry
(084) An unexpected overlap: A Case of Lupus Cerebritis, fevers, and mania in a patient with mixed connective tissue disease

Nia Harris, MD
Consultation-Liaison Psychiatry Fellow
New York-Presbyterian/Weill Cornell Medical Center
New York, New York
Jihoon Ha, MD
Assistant professor of clinical psychiatry
Weill Cornell Medical Center
New york, New York
Presenting Author(s)
Co-Author(s)
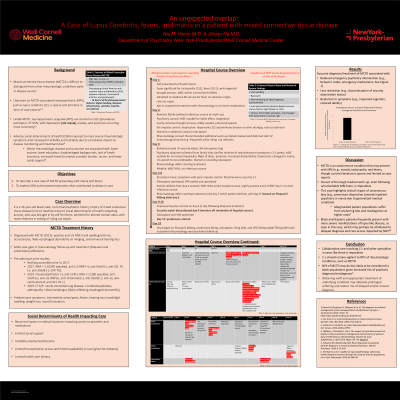
Background: Mixed connective tissue disease (MCTD) is characterized by overlapping features of systemic lupus erythematosus (SLE), scleroderma, myopathy, and arthritis.1 It can be difficult to distinguish from other rheumatologic conditions especially early on.1 Importantly, while neuropsychiatric sequalae (NPS) are common in SLE, they are rare in MCTD.2 Literature on MCTD-associated NPS, such as lupus cerebritis (LC), is sparse and primarily case reports.3-4 Here, we add to the limited body of literature and present a complex case of LC, fevers, and mania, as well as roles of race and social determinants of health (SDOH), in a patient with MCTD.
Case: X is a 39-year-old black male, no formal psychiatric history, history of MCTD (not on treatment due to SDOH impacting access), who was admitted for altered mental status with manic features in setting of ruling out sepsis. Exam was notable for digital swelling, acrosclerosis, sensorineural hearing loss, labile affect, disorganized thought process, flight of ideas, and irritability. Despite fevers, tachycardia, and elevated inflammatory markers, the primary team initially was concerned about primary psychiatric illness and strongly advocated for psychiatric admission. C-L psychiatry and rheumatology, however, insisted on a full medical work-up. This revealed negative blood cultures, negative brain magnetic resonance imaging, positive anti ribonucleoprotein and antiribosomal P protein antibodies, esophageal dysmotility, and nonspecific interstitial pneumonia, collectively consistent with MCTD. Despite these findings, medicine remained adamant that X’s symptoms resulted from “psychiatric disease.” However, after LP findings (mild pleocytosis and increased protein count), X was diagnosed with LC secondary to MCTD, accounting for fevers and mental status changes. X was started on hydroxychloroquine and prednisone. Olanzapine and valproate were titrated to target mania secondary to MCTD. X was stabilized and discharged with outpatient follow-up.
Discussion: Our case adds to limited literature and highlights a rare presentation of NPS, tachycardia, and fevers in MCTD. It also highlights the importance of thorough work-up, especially in marginalized populations, who are at increased risk of misdiagnosis.5 Moreover, Black and Hispanic patients frequently present with more severe manifestations of lupus-like disease, as seen in this case, which may perhaps be attributed to access and delayed diagnosis.6
Conclusion: In rare cases MCTD may present with unexpected symptoms (e.g. NPS). A collaborative approach, including exploration of treatment dynamics, in cases like this may alleviate prolonged suffering and ensure prompt, optimal treatment.
References:
1. Ortega-Hernandez OD, Shoenfeld Y. Mixed connective tissue disease: an overview of clinical manifestations, diagnosis and treatment. Best Pract Res Clin Rheumatol. 2012;26(1):61-72.
2. Nowicka-Sauer K et al. Neuropsychological assessment in mixed connective tissue disease: comparison with SLE. Lupus. 2012;21(9):927-933.
3. Lim JK et al. LC and steroid psychosis in mixed connective tissue disorder. Yale J Biol Med. 2004;77(3-4):63-9.
4. Leitao et al. Cerebritis as a Rare Neuropsychiatric Manifestation of SLE. Cureus. 2022;14(5):e24973.
5. Schwartz RC, Blankenship DM. Racial disparities in psychotic disorder diagnosis: A review of empirical literature. World J Psychiatry. 2014; 4:133-40.
6. Drenkard C, Lim SS. Update on lupus epidemiology: advancing health disparities research through the study of minority populations. Curr. Opin. Rheumatol. 2019;31:689–96
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Here we present a case in which a male from a historically marginalized background is inappropriately diagnosed as having a primary psychiatric condition despite ample evidence pointing towards an organic etiology. This case highlights the impact of conscious and unconscious bias related to race and social determinants of health on misdiagnosis. Moreover, we highlight the inequity that exists within severity of lupus-like disease presentation (i.e. persons from racially/ethnically minoritized backgrounds frequently present with more severe manifestations perhaps due to inequities in care access).

