Collaborative and Integrated Care
(047) Addressing the Consequences of Fertility Preservation Oversight in a Prostate Cancer Patient with Major Depressive Disorder: A Case Report

Yi Ling (Elaine) Li, MD
Assistant Professor
Icahn School of Medicine at Mount Sinai
Brooklyn, New York
Carrie L. Ernst, MD, FACLP
Associate Professor
Icahn School of Medicine at Mount Sinai
New Rochelle, New York
Presenting Author(s)
Co-Author(s)
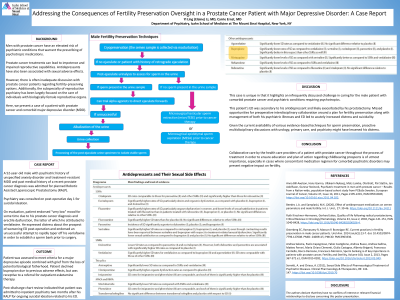
Background:
Men with prostate cancer have an elevated risk of psychiatric conditions that warrant the prescribing of psychotropic medications. Prostate cancer treatments, such as radical prostatectomy and chemotherapy, can lead to impotence and impaired reproductive capabilities. Antidepressants have also been associated with sexual adverse effects, including decreased libido, erectile dysfunction (ED), and delayed ejaculation. However, there is often inadequate discussion with prostate cancer patients regarding fertility-preserving options. Additionally, the subspecialty of reproductive psychiatry has been largely focused on the care of individuals with biologically female reproductive organs. Here, we present a case of a patient with prostate cancer and comorbid major depressive disorder (MDD), whose sexual dysfunction secondary to his antidepressant regimen and subsequent prostatectomy without an organized plan of fertility preservation by his providers led to suicidality and difficulty coping.
Case Report:
A 52-year-old male with psychiatric history of unspecified anxiety disorder and treatment-resistant MDD and past medical history of a recent prostate cancer diagnosis was admitted for planned Robotic Assisted Laparoscopic Prostatectomy (RALP).
Psychiatry was consulted on post-operative day 1 for suicidal ideation. On evaluation, patient endorsed "very low" mood for some time due to his prostate cancer diagnosis and ED, the latter of which he attributed to venlafaxine. He expressed distress about the prospect of worsening ED post-operation and endorsed an unsuccessful attempt to rapidly taper off his venlafaxine in order to establish a sperm bank prior to surgery. Patient was assessed to meet criteria for a major depressive episode combined with grief from the loss of potential biological fatherhood. Patient declined bupropion due to previous adverse effects, but was receptive to a referral for outpatient esketamine therapy. Post-discharge chart review indicated that patient was admitted to inpatient psychiatry two months after his RALP for ongoing suicidal ideation related to his ED.
Discussion:
This case is unique in that it highlights an infrequently discussed challenge in caring for the male patient with comorbid prostate cancer and psychiatric conditions requiring psychotropics. This patient’s ED was secondary to his antidepressant and likely exacerbated by his prostatectomy. Missed opportunities for preoperative interdisciplinary collaboration around a plan for fertility preservation along with management of both his psychiatric illnesses and ED led to acutely increased distress and suicidality. Given the current availability of various evidence-based techniques for sperm preservation, proactive multidisciplinary discussions with urology, primary care, and psychiatry might have lessened his distress.
Conclusion/Implications:
Collaborative care by the health care providers of a patient with prostate cancer throughout the process of treatment in order to ensure education and plan of action regarding childbearing prospects is of utmost importance, especially in cases where concomitant medication regimen for comorbid psychiatric disorders may present negative impact on fertility.
References:
Anna Bill-Axelson, Hans Garmo, Ullakarin Nyberg, et al, Psychiatric treatment in men with prostate cancer – Results from a Nation-wide, population-based cohort study from PCBaSe Sweden, European Journal of Cancer, 2011; 47: 2195-2201
Beeder, L.A. and Samplaski, M.K. Effect of antidepressant medications on semen parameters and male fertility. Int. J. Urol., 2020; 27: 39-46.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: The submission's primary author is a medical fellow. The subject matter to be presented involves the infrequently discussed topic of male sexual and reproductive health in the realm of psychiatry.

