Transplant Psychiatry and C-L Subspecialties
(207) Acute Psychosis Associated with Granulomatosis with Polyangiitis: A Case Discussion and Literature Review
- ET
Emma Torncello, MD
Psychiatry Resident
University of New Mexico
Albuquerque, New Mexico 
Samuel I. MacDonald, Medical Doctorate
Resident Physician
University of New Mexico
Albuquerque, New Mexico
William Wylie, MD
Consultation Liaison Psychiatry Fellow
University of New Mexico
Albuquerque, New Mexico
Davin Quinn, MD, FACLP (he/him/his)
Professor
University of New Mexico Health Sciences Center
Santa Fe, New Mexico
Presenting Author(s)
Co-Author(s)
Background:
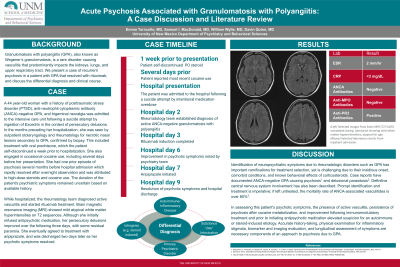
Granulomatosis with polyangiitis (GPA) is a rare disorder causing vasculitis that predominantly impacts the kidneys, lungs, and upper respiratory tract. We present a case of recurrent psychosis in a patient with GPA that resolved with rituximab, and review the differential diagnosis and treatment of psychosis in autoimmune disorders.
Case:
A 44 year-old woman with a history of posttraumatic stress disorder (PTSD), anti-neutrophil cytoplasmic antibody (ANCA)-negative GPA, and trigeminal neuralgia was admitted to the intensive care unit following a suicide attempt by ingestion of Excedrin in the context of persecutory delusions. In the months preceding her hospitalization, she was seen by outpatient otolaryngology and rheumatology for necrotic nasal lesions secondary to GPA, confirmed by biopsy. This included treatment with oral prednisone, which the patient self-discontinued a week prior to hospitalization. She also engaged in occasional cocaine use, including several days before her presentation. She had one prior episode of psychosis several months before which rapidly resolved after overnight observation and was attributed to high-dose steroids and cocaine use. The duration of the patient's psychiatric symptoms remained uncertain based on available history.
While hospitalized, the rheumatology team diagnosed active vasculitis and started rituximab treatment. Brain magnetic resonance imaging (MRI) showed mild atypical white matter hyperintensities on T2 sequences. Although she initially refused antipsychotic medication, her persecutory delusions improved over the following three days, with some residual paranoia. She eventually consented to treatment with aripiprazole, and was discharged two days later when her psychotic symptoms resolved.
Discussion:
Identification of neuropsychiatric symptoms due to rheumatologic disorders such as GPA has important ramifications for treatment selection, yet is challenging due to their insidious onset, comorbid conditions, and known behavioral effects of corticosteroids. Case reports have documented ANCA-negative GPA causing psychosis (Gasparinho et. al 2011) and delusional parasitosis (Schmoll 2011). Definitive central nervous system involvement has also been described. Prompt identification and treatment is imperative; if left untreated, the mortality rate of ANCA-associated vasculitides is over 80% (Yates & Watts 2017).
In assessing this patient's psychotic symptoms, the presence of active vasculitis, persistence of psychosis after cocaine metabolization, and improvement following immunomodulatory treatment and prior to initiating antipsychotic medication elevated suspicion for an autoimmune or steroid-induced etiology. Accurate history-taking, physical examination for inflammatory stigmata, biomarker and imaging evaluation, and longitudinal assessment of symptoms are necessary components of an approach to psychosis due to GPA.
Conclusion:
Our case outlines a multidisciplinary approach to management of acute psychosis with several potential etiologies and highlights features that may aid in identifying psychosis of autoimmune etiology.
References:
Gasparinho, R., Fernandes, N., Martins, M., Santos, N., Ferreira, L. P., & Alho, A. (2022). Psychosis as the First Manifestation of Granulomatosis with Polyangiitis - A Case Report. Psychiatria Danubina, 34(2), 315–317.
Schmoll D. (2011). Sekundärer Dermatozoenwahn bei Wegener Granulomatose [Delusion of parasitosis due to Wegener's granulomatosis]. Fortschritte der Neurologie-Psychiatrie, 79(4), 234–237.
Yates M, Watts R. ANCA-associated vasculitis. Clin Med (Lond). 2017 Feb;17(1):60-64. doi: 10.7861/clinmedicine.17-1-60. PMID: 28148583; PMCID: PMC6297586.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Our case is a reminder of the importance of maintaining a broad differential when approaching a patient with psychiatric complaints. Certain populations, especially patients from marginalized communities, patients experiencing homelessness, and patients with substance use disorders may not receive adequate medical workup for acute changes in behavior and cognition in the context of rheumatologic disease. In our case, what initially appeared to be an incidental finding (a necrotic nasal lesion) proved vital for this patient’s treatment and positive outcome, and is an example of multidisciplinary teamwork overcoming potential biases and confounding psychosocial factors.

