Women's Mental Health
(223) A Systematic Review of the Impact of Study Methodology Upon Findings Regarding the Relationship Between Breastfeeding & Postpartum Depression
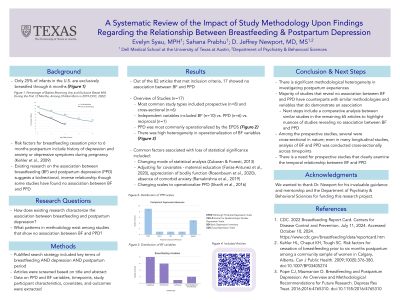
Evelyn Syau, MPH
Medical Student
The University of Texas at Austin - Dell Medical School
Austin, Texas
Sahana Prabhu, n/a
Medical Student
Dell Medical School
Flower Mound, Texas
Presenting Author(s)
Co-Author(s)
Background/Significance
The association between breastfeeding (BF) and postpartum depression (PPD) has been extensively investigated, with the majority of studies suggesting a bidirectional, inverse relationship between the two variables. However, a fraction of studies have found no association between BF and PPD, a conclusion that contradicts what is predominately established in the literature as well as clinical anecdotes. Our objective is to highlight methodological patterns in studies finding no association between BF and PPD and ultimately, differences with studies that do. Methods Our PubMed search strategy, which included key terms of breastfeeding AND depression AND postpartum period, yielded 2,688 articles. Two independent reviewers screened the articles based on titles and abstracts. Out of this initial screen, 82 articles fulfilled criteria for data extraction. Particular attention was paid to methodologies, timepoints, PPD and BF operationalization, and statistical significance of association. A review was then conducted for the articles demonstrating no association. Results Out of the 82 articles, 17 showed no association between BF and PPD. The most common study types were prospective (n=8) and cross-sectional (n=6). Ten and six articles examined BF and PPD as independent variables, respectively, and one examined the variables reciprocally. PPD was operationalized most commonly with the EPDS alone (n=8) and in tandem with other scales (n=2). BF variables were either categorical (n=8) (practices, difficulties), dichotomous (n=6) (initiation, cessation), continuous (n=1) (duration), and mixed categorical and continuous (n=2). Several studies lost statistical significance when accounting for covariates, such as appreciation of bodily function (Rosenbaum et al., 2020) and maternal education (Farías-Antúnez et al., 2020). Others only found statistical significance at certain time points (Galler et al., 2006). The remaining articles postulated reasons for this lack of association, but did not specifically investigate these factors. Discussion The precise nature of BF and PPD remains elusive. This is due to significant methodological variability and heterogeneity in postpartum experiences, which is not consistently accounted for by existing research. Still, most studies confirm the two are associated. The majority of studies revealing no association between BF and PPD have counterparts with similar methodologies and variables that do demonstrate an association. Our next steps include a comparative analysis between similar studies in the remaining 65 to highlight nuances of studies revealing no association between BF and PPD. Conclusion To clarify the association between BF and PPD, more robust, prospective studies with clear postpartum timepoints and continuous and/or categorical BF variables should be conducted. This echoes Pope and Mazmanian’s 2016 piece suggesting similar methodological recommendations for future research. Importantly, refining the relationship between BF and PPD can further inform clinical recommendations about BF in the context of PPD. References Pope CJ, Mazmanian D. Breastfeeding and Postpartum Depression: An Overview and Methodological Recommendations for Future Research. Depress Res Treat. 2016;2016:4765310. doi:10.1155/2016/4765310
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Postpartum depression (PPD) is one of the leading causes of morbidity and mortality in the postpartum period with outcome disparities across race, ethnicity, SES, and region. PPD is associated with decreased breastfeeding outcomes, which can subsequently impact infant health and mother/child bonding. Conversely, breastfeeding pressures and difficulties may disproportionately affect those who face other psychosocial stressors, contributing to PPD. Thus, clarifying the relationship between breastfeeding and PPD can allow for more directed efforts towards reducing disparities observed in PPD outcomes as well as access to maternal mental healthcare.

