Catatonia
(022) ECT Treatment for Catatonia Post Liver Transplant
- SB
Sarah J. Beneteau, RN-EC, PHC-NP (she/her/hers)
Nurse Practitioner, Psychiatry
University Health Network, University of Toronto
Toronto, Ontario, Canada .jpg)
Adrienne Tan, FACLP
C-L Psychiatrist and Medical Lead, Medical Psychiatry
University of Toronto
Toronto, Ontario, Canada.jpg)
Kathleen Sheehan, MD, DPhil
Associate Professor
University of Toronto
Toronto, Ontario, Canada- DK
Dilip Koshy, FRCPC
Staff psychiatrist
University of Toronto, Temerty Faculty of Medicine
Toronto, Ontario, Canada .jpg)
Suze Berkhout, MD/PhD, FRCPC
Clinician Investigator
University Heath Network
Toronto, Ontario, Canada- NA
Noha Abdel Gawad, MD,ABPN,FRCPC
Assistant Professor
University of Toronto
Toronto, Ontario, Canada - RS
Rickinder Sethi, MD
Lecturer and Staff Psychiatrist
University of Toronto
Toronto, Ontario, Canada - cT
cynthia Tsien, MDCM
Assistant Professor
Toronto General Hospital
Toronto, Ontario, Canada - LA
Laia Aceituno sierra, n/a
Clinical Fellow
University of Toronto
Toronto, Ontario, Canada - CW
Caitlin White, RN(EC), MN, Adult-NP
Nurse Practitioner
University Health Network - Toronto General Hospital
Toronto, Ontario, Canada
Presenting Author(s)
Co-Author(s)
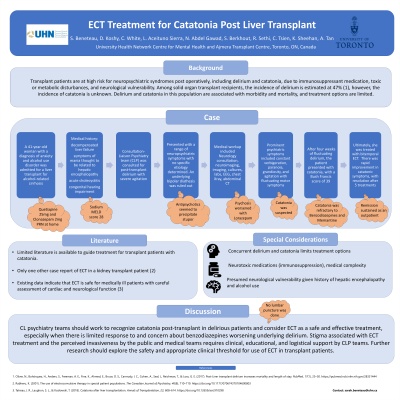
Background:
Transplant patients are at risk for neuropsychiatric syndromes, including delirium and catatonia, due to immunosuppressant medication, toxic or metabolic disturbances, and neurological vulnerability. Among solid-organ transplant patients, the incidence of delirium is estimated at 47% (Oliver et. al., 2017), however, the incidence of catatonia is unknown. Delirium and catatonia in this population are associated with morbidity and mortality, and treatment options are limited. Herein, we report a case of a liver transplant recipient with delirium and catatonia refractory to treatment with benzodiazepines successfully treated with Electroconvulsive therapy (ECT).
Case:
A 41-year-old woman with a diagnosis of anxiety and alcohol use disorder was admitted for liver transplant for alcohol-associated cirrhosis, with a MELD-Na score of 28. Psychotropic medications included Clonazepam 0.5mg and Quetiapine 25mg as needed at bedtime. Medical history was notable for decompensated liver failure with symptoms of mania thought to be related to hepatic encephalopathy, acute cholecystitis and congenital hearing impairment. The Consultation-Liaison Psychiatry team (CLP) was involved for delirium with severe agitation, initially treated with antipsychotics, with intermittent doses of Ativan. The patient presented with a range of neuropsychiatric symptoms with no specific etiology determined. Her psychiatric history was reviewed to rule out an underlying bipolar diathesis. Tacrolimus levels remained within normal limits. The patient subsequently presented with catatonia, with a Bush Francis score of 39. Catatonia was refractory to benzodiazepines and Memantine and she was treated with 5 sessions of bilateral ECT. There was rapid improvement in catatonic symptoms, and she was discharged home after 5 sessions. She sustained remission as an outpatient.
Discussion:
Limited literature is available to guide treatment for transplant patients with catatonia. Case reports focus on catatonia which responded to benzodiazepines, with one other case report of ECT in a kidney transplant patient (Tatreau, Laughon, & Kozlowski, 2018). Existing data indicate that ECT is safe for medically ill patients (Rabheru 2001); however, more recent and controlled data are limited. In this case, bilateral ECT was safely used to treat a liver-transplant patient with catatonia with no adverse effects to date. Interprofessional and family support was essential in planning and delivering ECT safely.
Conclusions/Implications:
CL psychiatry teams should work to recognize catatonia post-transplant in delirious patients and consider ECT as a safe and effective treatment, especially when there is concern about benzodiazepines worsening underlying delirium. Stigma associated with ECT treatment requires clinical, educational, and logistical support by CLP teams. Further research should explore the safety and appropriate clinical threshold for use of ECT in transplant patients.
References:
Oliver, N., Bohórquez, H., Anders, S., Freeman, A. E., Fine, K., Ahmed, E., Bruce, D. S., Carmody, I. C., Cohen, A., Seal, J., Reichman, T., & Loss, G. E. (2017). Post-Liver transplant delirium increases mortality and length of stay. PubMed, 17(1), 25–30. https://pubmed.ncbi.nlm.nih.gov/28331444
Rabheru, K. (2001). The use of electroconvulsive therapy in special patient populations. The Canadian Journal of Psychiatry, 46(8), 710–719. https://doi.org/10.1177/070674370104600803
Tatreau, J. R., Laughon, S. L., & Kozłowski, T. (2018). Catatonia after liver transplantation. Annals of Transplantation, 23, 608–614. https://doi.org/10.12659/aot.910298
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Safety data focusing on ECT post-transplant may eliminate some barriers to transplant for those with serious mental illness. Work by CLP teams in this area can reduce stigma associated with transplanting patients who have a history of treatment with ECT or who may require ECT post-transplant.

