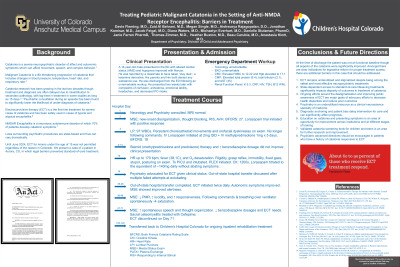
Neurocognitive Disorders and Neuropsychiatry
(104) Treating Pediatric Malignant Catatonia In The Setting Of Anti-NMDA Receptor Encephalitis: Barriers In Treatment

Davis Fleming, MD (he/him/his)
Child and Adolescent Psychiatry Fellow PGY5
University of Colorado-Anschutz Medical Campus
Aurora, Colorado- AZ
Al-Bahrani Zaid, M.D.
PGY-2
University of Colorado
Denver, Colorado - BH
Buxton Heather, MD
Senior Instructor
University of Colorado
Denver, Colorado 
Megan Single, MD
Fellow Physician
Duke University
Morrisville, North Carolina
Danielle L. Stutzman, PharmD, BCPP
Psychiatric Pharmacist
Pediatric Mental Health Institute, Children's Hospital Colorado
Denver, Colorado- JF
Janie Ferren, PharmD, BCPP
Clinical Pharmacy Specialist
Pediatric Mental Health Institute, Children's Hospital Colorado
Denver, Colorado - ME
Michaelyn Everhart, MD
Fellow Physician PGY-4
University of Colorado
Denver, Colorado 
Beau A. Carubia, Medical Doctor (MD)
Assistant Professor
University of Colorado School of Medicine
Aurora, Colorado
Anastasia Klott, MD
Assistant Professor
Children's Hospital Colorado
Aurora, Colorado- JF
Jacob Feigal, MD
Assistant Professor
Duke University Medical School
Durham, North Carolina 
Thomas Zimmer, MD
Senior Instructor
University of Colorado
Aurora, Colorado
Aishwarya Rajagopalan, D.O.
Pediatric Consultation Liaison Psychiatrist
Duke University School of Medicine
Durham, North Carolina- JK
Jonathan R. Komisar, MD
Assistant Professor
Duke University School of Medicine
Durham, North Carolina - DW
Diana Waters, MD
Research Resident
Duke University
Durham, North Carolina
Presenting Author(s)
Co-Author(s)
Catatonia is a severe neuropsychiatric disorder which can affect movement, speech, and complex behavior, often in conjunction with affective and autonomic symptoms (Rogers et al 2023). Catatonia can exist as a primary condition or secondary to a medical condition such as autoimmune encephalitis (Connell et al 2023). Malignant catatonia describes catatonia which presents with significant autonomic dysfunction, including changes in blood pressure, heart rate, respiratory rate, and temperature (Connell et al 2023). Catatonia carries a 60-fold increase in premature death in adolescent populations (Benarous et al 2018). It has been estimated that inflammatory brain disorders contribute as underlying medical disorders in up to 28% of patients with catatonia (Oldham et al. 2018). Moreover, approximately 70% of young patients with autoimmune neuropathology, specifically anti-N-methyl-D-aspartate receptor (anti-NMDAR) encephalitis, develop catatonic symptoms (Benarous et al 2018). Anti-NMDAR encephalitis is a systemic autoimmune disorder with severely neurotoxic effects, and the presence of catatonia in this setting constitutes “severe disease” (Coffey et al. 2016, Nosadini et al 2021). Although catatonia research has been growing for the last two decades, its recognition and treatment continues to be delayed through misattribution to secondary pathology (Reinfield and Gill 2022). The current literature surrounding treatment for this severe presentation is limited to heterogenous case reports and series (Rogers et al. 2023). Electroconvulsive therapy (ECT) has been shown to be a safe and effective treatment for catatonia, and it has been safely used in cases of typical and atypical encephalitis, targeting both seizures and symptoms of catatonia (Coffey et al. 2016). ECT may play an important role in treating adolescents with malignant catatonia secondary to anti-NMDAR encephalitis (Coffey et al. 2016). However, certain states have legislation which prevent minors from receiving this life-saving treatment. We present a case of a 14-year-old male with malignant catatonia secondary to confirmed anti-NMDAR encephalitis that highlights systemic obstacles, legislative barriers, and diagnostic overshadowing to his treatment and outcome. We discuss the clinical implications, ramifications for reform and advocacy, and areas of future research related to this case.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: In this case, we discuss the systemic and legislative barriers that prevented urgent care in an adolescent of a minority population. We discuss the inequity of care seen in this population due to these barriers and diagnostic overshadowing. We believe systemic reform is crucial to remove legislative barriers and diagnostic overshadowing which continue to negatively affect these marginalized populations.

