Psychopharmacology and Toxicology
(136) Clozapine Related Cecal Volvulus
- SB
Sharlo Bayless, MD / MS
Psychiatry Resident
Jacobs School of Medicine SUNY Buffalo
Buffalo, New York - RL
Raphael Jerome Leo, MD, FACLP
Director, Consultation Liaison Service at ECMC
Jacobs School of Medicine SUNY Buffalo
Buffalo, New York
Presenting Author(s)
Co-Author(s)
Background:
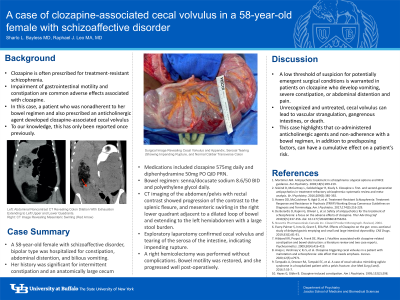
Impairment of gastrointestinal motility is a common side effect of clozapine. Serious complications can result, including paralytic ileus, obstruction, gastrointestinal ischemia, and death (Every-Palmer 2019). Here we describe a case of cecal volvulus associated with clozapine use. To our knowledge, clozapine-related cecal volvulus has only been reported once previously (Aneja 2020). This case illustrates the need to be watchful of surgical emergencies in clozapine-treated patients.
Case:
A 58-year-old female with schizoaffective disorder, residing in a long-term psychiatric facility, was hospitalized for constipation, abdominal distention, and bilious vomiting lasting 3 days. Her psychiatric medications included clozapine 575mg daily. Diphenhydramine 50mg PO QID PRN was recently initiated for pruritis. She was non-adherent with her bowel regimen of senna/docusate sodium and polyethylene glycol and her bowel habits were not documented. Despite her advanced age and lack of an intimate partner, she had a delusional belief that the symptoms were from pregnancy.
An abdominal x-ray revealed dilation of the colon containing an air-fluid level of the left upper and lower quadrants with preservation of haustral folds. The initial clinical impression was Ogilvie syndrome. Clozapine and diphenhydramine were withheld. An aggressive bowel regimen was suggested, but the patient refused it as she insisted she was pregnant.
Computerized technology (CT) imaging of the abdomen/pelvis showed progression of rectal contrast to the splenic flexure and mesenteric swirling in the right lower quadrant. Cecal volvulus was suspected. Exploratory laparotomy confirmed cecal volvulus and intestinal serosa tearing, which indicated impending rupture. A right hemicolectomy with stapled side-to-side anastomosis was performed without complications. She progressed well post-operatively and returned to her facility.
Discussion:
The anticholinergic, serotonergic and noradrenergic effects of clozapine are implicated in the hypomotility side effects (Aneja 2020). For clozapine-treated patients developing abdominal pain and distention, vomiting, and constipation, a careful work-up is warranted.
Cecal volvulus is related to improper fusion of the cecal mesentery with the retroperitoneum, predisposing the cecum to rotation. CT imaging of the patient’s abdomen 4 years earlier revealed a large, antero-medially oriented, and mobile cecum. Exacerbated by an increased anticholinergic burden from diphenhydramine and non-adherence with the bowel regimen, she was vulnerable to developing cecal volvulus.
Conclusion:
Psychiatrists enlisted in the care of patients receiving clozapine need to retain a low threshold of suspicion for potentially emergent conditions associated with severe constipation. Providers should also exercise caution for patients with predisposing factors such as unusual bowel anatomy. Patients taking clozapine require diligent documentation of bowel habits, adherence with bowel management, and a reduced anticholinergic burden to mitigate risks.
References:
Every-Palmer S, Inns SJ, Grant E, Ellis PM. Effects of Clozapine on the gut: cross-sectional study of delayed gastric emptying and small and large intestinal dysmotility. CNS Drugs. 2019;33(1):81-91. doi: 10.1007/s40263-018-0587-4.
Aneja J, Varshney V, Ks S, et al. Clozapine triggering cecal volvulus in a patient with malrotation and schizophrenia: side effect that needs emphasis. Cureus. 2020;12(5):e7971. doi: 10.7759/cureus.7971.
Presentation Eligibility: This case report was submitted to Primary Care Companion for CNS Disorders. We have not heard back regarding whether it will be accepted. There is benefit to presenting at this meeting because CL psychiatrists might be enlisted to follow patients with rare surgical complications that result from psychotropic medications.
Diversity, Equity, and Inclusion: This submission demonstrates the need to be attentive to life-threatening side effects from psychotropic medications in patients with severe schizophrenia. These patients, who often reside in long-term psychiatric facilities, may not be able to adequately explain their symptoms or advocate for their needs. Our case report could advance equity for these patients by encouraging physicians to be more watchful of medical and surgical emergencies in this population.

