Collaborative and Integrated Care
(051) Cardiovascular risk profiles of primary care patients eligible for collaborative care for depression and anxiety
- ZB
Zachary Bean, MD (he/him/his)
Fellow
Northwestern Medicine
Chicago, Illinois - AC
Allison J. Carroll, PhD
Research Assistant Professor
Northwestern University Feinberg School of Medicine
Chicago, Illinois - SP
Sarah E. Philbin, MPH
PhD Candidate
Northwestern University
Chicago, Illinois - HP
Havisha Pedalluma, BA
Medical Student
Feinberg School of Medicine
Chicago, Illinois 
Saneha Borisuth, n/a
Medical Student
University of Illinois College of Medicine
Chicago, Illinois- OS
Olutobi A. Sanuade, n/a
Research Assistant Professor
University of Utah
Salt Lake City, Utah - EF
Emily Fu, MPH, MS
Clinical Psychology Doctoral Candidate
Northwestern University Feinberg School of Medicine
Chicago, Illinois 
Lisa Rosenthal, MD, FACLP
Professor
Northwestern University
chicago, Illinois- JR
Jeffrey Rado, MD, MPH, FAPA
Associate Professor
Northwestern University Feinberg SOM
Chicago, Illinois - CB
C. Hendricks Brown, PhD
Professor
Feinberg School of Medicine Northwestern University
Chicago, Illinois 
Justin D. Smith, PhD
Associate Professor
University of Utah Spencer Fox Eccles School of Medicine
Salt Lake City, Utah
Presenting Author(s)
Co-Author(s)
Background/Significance:
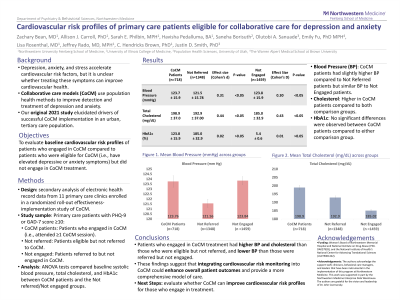
Collaborative care models (CoCM) have been found to improve the detection of depression and anxiety, and patient access to behavioral health providers. Recent studies have shown depression, anxiety, and stress to accelerate progression of cardiovascular risk factors (Fu et al 2023). In this study, we examined the baseline cardiovascular risk profiles of patients who were eligible for CoCM for depression or anxiety. This secondary analysis used electronic health record data from 11 primary care clinics at Northwestern Medicine that were enrolled in a randomized roll-out type 2 hybrid effectiveness-implementation study. Eligibility for CoCM required a PHQ-9 or GAD-7 ≥10. The study sample included patients who were eligible and engaged in CoCM (i.e., attended at least 1 session; Intervention group), patients who were eligible for CoCM and not referred (Comparison 1 group), and patients who were referred to CoCM but did not engage in treatment (Comparison 2 group). We used ANOVAs to examine baseline differences in systolic blood pressure (BP), total cholesterol, and HbA1c between the intervention and comparison groups. There were a total of 718 patients in the Intervention group, 1348 in Comparison 1, and 1459 in Comparison 2. Mean BP in the intervention group was 123.76±15.90 mmHg, compared to 121.56±15.78 mmHg in Comparison 1 (p< .05, d=0.31) and 123.84±15.92 mmHg in Comparison 2 (p< .05; d=0.30). Mean total cholesterol in the intervention group was 198.90±37.00 mg/dL, compared to 192.90±37.00 mg/dL in Comparison 1 (p< .05, d=0.44) and 185.02±32.99 mg/dL in Comparison 2 (p< .05, d=0.43). Mean HbA1c in the intervention group was 6.17±1.59%, compared to 5.24±0.21% in Comparison 1 (p>.05, d=0.02) and 5.43±0.66% in Comparison 2 (p>.05, d=0.01). Notably, the proportion of the Intervention sample with BP and cholesterol was less than in either Comparison group, while the group proportions with HbA1c were comparable. The baseline cardiovascular risk profiles of patients eligible to engage in CoCM treatment were mixed. The group of patients who ultimately engaged in CoCM treatment had higher BP and cholesterol than those who were eligible and not referred, and lower BP and higher cholesterol than those who were referred but not engaged. No group differences were observed in HbA1c. Conclusion/Implications: This was the first study to our knowledge to examine the cardiovascular risk profiles of individuals who were eligible for CoCM treatment (i.e., had elevated depressive or anxiety symptoms) but who may or may not have engaged in treatment. The next step for this study will be to evaluate whether CoCM treatment can improve the cardiovascular risk profiles of those who engaged in treatment compared to those who did not. Fu, E., Carroll, A. J., Rosenthal, L. J., Rado, J., Burnett-Zeigler, I., Jordan, N., Carlo, A. D., Ekwonu, A., Kust, A., Brown, C. H., Csernansky, J. G., & Smith, J. D. (2023). Implementation Barriers and Experiences of Eligible Patients Who Failed to Enroll in Collaborative Care for Depression and Anxiety. Journal of general internal medicine, 38(2), 366–374. https://doi.org/10.1007/s11606-022-07750-8
Methods:
Results:
Discussion:
References:
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Racial disparities are pervasive in mental health conditions, cardiovascular disease, and access to healthcare. Collaborative care (CoCM) is designed to improve access to mental health services by offering integrated treatment in primary care settings. If we find in our ongoing work that CoCM can effectively and equitably improve cardiovascular risk profiles for individuals who engage in CoCM for depression and anxiety, this will lend evidence to support CoCM as an evidence-based approach for advancing health equity.

