Transplant Psychiatry and C-L Subspecialties
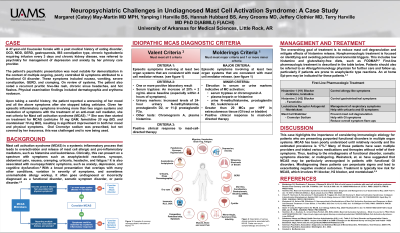
(215) Mast Cell Activation Syndrome (MCAS), Demoralization and Escalating Anxiety; A Case Report.

Margaret (Catey) May, MD MPH (she/her/hers)
Resident
University of Arkansas for Medical Sciences
Little Rock, Arkansas- HH
Hannah Hubbard, BS
Medical Student
UAMS
Little Rock, Arkansas - YH
Yanping I. Harville, n/a
MD-PhD Student
UAMS
Little Rock, Arkansas 
Amy Grooms, MD
Assistant Professor
UAMS
Little Rock, Arkansas- JC
Jeffery Clothier, MD
Professor
University of Arkansas for Medical Sciences
Little Rock, Arkansas - TH
Terry Harville, MD PhD D(ABMLI) F(ACHI)
Professor / Medical Director
University of Arkansas for Medical Sciences
Little Rock, Arkansas
Presenting Author(s)
Co-Author(s)
Background: Mast cell activation syndrome (MCAS) is a systemic inflammatory process that leads to overactivation and release of mast cell pro-inflammatory mediators, such as histamine. Clinically, this can present on a spectrum with symptoms such as anaphylaxis, syncope, abdominal pain, nausea, cramping, urticaria, headache, and fatigue (Valent, 2022). It is also associated with neuropsychiatric symptoms, such as anxiety, depression, and cognitive dysfunction (Weinstock, 2023). With a broad presentation that overlaps with many other conditions and variations in the severity of symptoms, it often goes undiagnosed or incorrectly diagnosed as a functional disorder (Hamilton, 2024).
Case: Herein, we present a case of a 47-year-old Caucasian female, Ms. R, with a past medical history of eating disorder, OCD, MDD, GERD, gastroparesis, IBS constipation type, chronic hypokalemia requiring infusion every 3 days and CKD, who was referred to psychiatry for management of depression and anxiety by her primary care provider.
Ms. R’s psychiatric presentation was most notable for demoralization in the context of multiple ongoing, poorly controlled GI symptoms attributed to a functional GI disorder. These symptoms included nausea, vomiting, severe constipation, GERD, and cramping. On review of systems, Ms. R also endorsed a recurrent pruritic hive-like rash, chronic sinus headaches, and hot flashes. Physical exam findings included dermatographia and erythema nodosum. Upon taking a careful history, the patient reported a worsening of her mood and all the above symptoms after she stopped taking cetirizine. Given her episodic inflammatory symptoms involving more than two organ systems and resolution of symptoms with treatment of an anti-mast cell mediator, she met criteria for MCAS (Valent, 2022), (Hamilton, 2024). She was then started on treatment for MCAS, resulting in significant improvement in both her mood and physical symptoms.
Discussion: This case highlights the importance of considering immunologic etiology for patients who are presenting purported functional disorders in multiple organ systems. MCAS has been poorly understood until relatively recently and the estimated prevalence is 17% (Hamilton, 2024). Weinstock, et. al. have suggested that MCAS may be particularly unrecognized in patients with functional GI disorders. Treatment typically involves H1 blocker, H2 blocker and montelukast, and is of low risk.
Conclusion: For patients with functional gastrointestinal disorders and resulting demoralization, it is important for psychiatrist to consider Mast Cell Activation Syndrome (MCAS). Treatment is typically of low-risk and can offer significant improvement in quality of life.
References:
1. Valent P, Hartmann K, Bonadonna P, Niedoszytko M, Triggiani M, Arock M, Brockow K. Mast Cell Activation Syndromes: Collegium Internationale Allergologicum Update 2022. Int Arch Allergy Immunol. 2022;183(7):693-705. doi: 10.1159/000524532. Epub 2022 May 23. PMID: 35605594; PMCID: PMC9393812.
2. Weinstock LB, Nelson RM, Blitshteyn S. Neuropsychiatric Manifestations of Mast Cell Activation Syndrome and Response to Mast-Cell-Directed Treatment: A Case Series. J Pers Med. 2023 Oct 31;13(11):1562. doi: 10.3390/jpm13111562. PMID: 38003876; PMCID: PMC10672129.
3. Hamilton MJ. Mast Cell Activation Syndrome and Gut Dysfunction: Diagnosis and Management. Curr Gastroenterol Rep. 2024 Feb 14. doi: 10.1007/s11894-024-00924-w. Epub ahead of print. PMID: 38353900.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: This submission seeks to develop the knowledge base of CL psychiatrists to further advocate for equitable healthcare of patients with a history of mental illness. With regards to author and co-author demographics, this poster represents diversity in career stages, ranging from a first-year medical student to practicing physicians.

