Psychotherapy and Non-Pharmalogic Interventions
(157) Shedding Light on Hypersomnia: A Case of Hepatobiliary Pathology in a Psychiatric Context
.jpg)
Laura Marengo, MD (she/her/hers)
Psychiatrist
Massachusetts General Hospital
Boston, Massachusetts- SM
Sarah MacLaurin, PMHNP
psychiatric nurse practitioner
MGH
Boston, MA, Massachusetts .jpg)
Scott Beach, MD, FACLP
Psychiatrist
Massachusetts General Hospital
Boston, Massachusetts- JR
Judith Restrepo, MD
Co-Director Transplant Psychiatry
Mass General Hospital
Boston, Massachusetts
Presenting Author(s)
Co-Author(s)
Background: Consultation-liaison psychiatrists must remain vigilant for medical causes of hypersomnia. Reflexively attributing hypersomnia to psychopathology or psychotropics can lead to ineffective or exacerbating interventions. Here, we present a case of hypersomnolence due to hepatobiliary pathology in a patient with schizophrenia and catatonia, on clozapine and benzodiazepines, managed effectively with lightbox therapy.
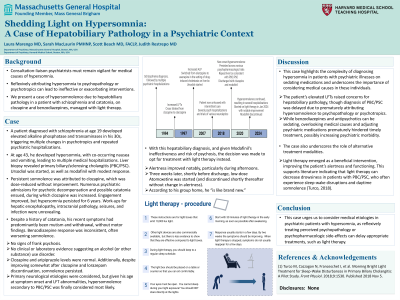
Case: A patient with schizophrenia since age 19 developed elevated alkaline phosphatase and transaminases in his 30s, triggering multiple changes in psychiatric medication and repeated psychiatric hospitalizations. At age 43, he developed hypersomnia, with co-occurring nausea and vomiting, leading to multiple medical hospitalizations. Liver biopsy revealed primary biliary/sclerosing cholangitis (PBC/PSC). Modafinil was started with modest response.
Persistent somnolence was subsequently attributed to clozapine, which was dose-reduced without significant improvement. Numerous psychiatric admissions for psychotic decompensation and possible catatonia ensued. Engagement improved with clozapine increase, but hypersomnia persisted.
At age 49, he presented with thrombocytopenia, hypothermia, hypoglycemia, and worsening somnolence. Work-ups for hepatic encephalopathy, intracranial pathology, seizures, and infection were unrevealing.
At various times, the hypersomnolence was attributed to catatonia, psychosis, substance use, and psychotropics. Despite a history of catatonia, his recent symptoms had predominantly been mutism and withdrawal, without motor findings. Benzodiazepine response was inconsistent, often worsening somnolence, lowering suspicion. There was no clinical or laboratory evidence suggesting an alcohol (or other substance) use disorder. He was without signs of frank psychosis. Clozapine and aripiprazole levels were normal. Additionally, despite improving somewhat after clozapine and lorazepam discontinuation, somnolence persisted. Primary neurological etiologies were also considered, but given his age at symptom onset and LFT abnormalities, hypersomnolence secondary to PBC/PSC was considered most likely.
With this diagnosis, and given Modafinil's ineffectiveness and risk of psychosis, the decision was made to start morning light therapy instead. Alertness improved notably, particularly during afternoons. Weeks later, shortly before discharge, low-dose Atomoxetine was started (and has not been increased). According to reports from his group home, he “is like brand new.”
Discussion: This case highlights the complexity of diagnosing hypersomnia in patients with psychiatric illnesses on sedating medications and underscores the importance of considering medical causes in these individuals. In this case, elevated LFTs raised concerns for hepatobiliary pathology, though diagnosis of PBC/PSC was delayed due to reflexively attributing hypersomnolence to psychopathology or psychotropics. While medications like benzodiazepines and antipsychotics can be sedating, adjusting psychiatric medications prematurely and overlooking medical causes hindered timely treatment, possibly increasing psychiatric morbidity.
The case also underscores the role of alternative treatment modalities. Light therapy emerged as a beneficial intervention, improving alertness and functioning. This supports literature indicating that light therapy can decrease drowsiness in patients with PBC/PSC, who often experience sleep-wake disruptions and daytime somnolence (Turco, 2018).
Conclusion: This case urges us to consider medical etiologies in psychiatric patients with hypersomnia, as reflexively treating perceived psychopathology or psychopharmacologic side-effects can delay appropriate treatments, such as lightbox therapy.
References: Turco M, Cazzagon N, Franceschet I, et al. Morning Bright Light Treatment for Sleep-Wake Disturbances in Primary Biliary Cholangitis: A Pilot Study. Front Physiol. 2018;9:1530. Published 2018 Nov 5.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: This case report highlights the intersectionality of medical and psychiatric conditions, which is often and especially overlooked in marginalized populations (which was likely a contributing factor for the patient in question, although not explicitly discussed in the abstract due to length limitations). By elucidating the diagnostic challenges faced by individuals with schizophrenia, the case underscores disparities in healthcare access and diagnostic delays, showcasing the need for vigilance in recognizing medical causes of hypersomnia in diverse patient populations. By promoting awareness of these complexities, the presentation contributes to more equitable and inclusive healthcare practices, fostering better outcomes for marginalized individuals.

