Neurocognitive Disorders and Neuropsychiatry
(091) Filling the Gap: An Innovative Approach to Autoimmune Encephalitis Using an Index-of-Suspicion Model

Jeanie Kim, BA
Medical Student
Loma Linda University School of Medicine
Loma Linda, California- MA
Mark D. Ard, Jr, MD, MA
Staff Psychiatrist
Loma Linda VA Hospital
Loma Linda, California - MA
Matthew Allen, MD
Resident Physician
Loma Linda University Health
Loma Linda, California 
My Phuong Tong, MD
Resident Psychiatrist
Loma Linda University
Redlands, California
Presenting Author(s)
Co-Author(s)
Background/Significance:
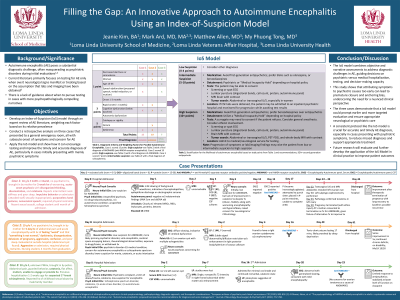
Autoimmune encephalitis (AE) poses a substantial diagnostic challenge, often masquerading as a psychiatric disorder upon initial evaluation.1,2 Current guidelines mainly focus on overt neurological signs, leaving a void for cases with psychopathologically compelling narratives, where systematic evaluation of evidence-based factors is particularly key.3 This study introduces an innovative "index-of-suspicion" (IoS) framework to ensure timely and appropriate diagnosis and care.
Methods:
The IoS model was developed through expert review of AE literature, weighting each factor based on the relative prevalence. A retrospective analysis was conducted on three cases that presented to a general emergency room, all with subacute onset of symptoms and concern for potential AE that was not investigated initially. The IoS model was retrospectively applied to these cases to highlight how attributing symptoms to psychiatric etiology can lead to premature closure and anchoring bias.
Results:
A collaborative, multidisciplinary approach emerged as crucial for thorough evaluation, accurate diagnosis, and prompt initiation of definitive treatment in AE cases. A model stratifying patents based on indicators such as rapidity of onset, age range, cognitive dysfunction, and seizure activity emerged. Low-suspicion cases (0-4 points) prompt alternative diagnoses. Intermediate cases (5-10 points) should avoid potent dopamine blockers, and attempts should be made to test cerebrospinal fluid. However, they can be observed in an inpatient psychiatric unit, monitoring for symptom progression and/or awaiting lab work. High-suspicion cases (10+ points) should prioritize benzodiazepines over antipsychotics, and diagnostic tests should be performed before considering inpatient psychiatric treatment, which may require special institutional tools for medical detainment and surrogate consent. Tests for intermediate- and high-suspicion cases include abdominal or transvaginal ultrasound, routine EEG, cerebrospinal fluid analysis, and brain MRI with contrast. Importantly, the model recognizes AE's dynamic nature, allowing for reclassification based on symptom progression and new findings.
Discussion:
Combining objective and narrative evaluations, the IoS model addresses practical and logistical challenges in AE diagnosis, guiding decisions on psychiatric versus medical hospitalization, diagnostic testing, and determination of decision-making capacity. The study underscores the importance of avoiding premature attribution of symptoms to psychiatric etiologies, advocating instead for a nuanced clinical perspective. The model is presented alongside case studies to show how using IoS classification would have prompted earlier and more directed evaluation and treatment and appropriate disposition to neurological versus psychiatric services.
Conclusion/Implications:
The IoS model offers clinicians a structured approach to AE detection, minimizing missed diagnoses and facilitating timely intervention. Future research will assess its effectiveness, emphasizing ongoing development for clinical education and practice to enhance diagnostic accuracy and patient outcomes.
References:
- Endres, Dominique, et al. "Autoimmune encephalitis as a differential diagnosis of schizophreniform psychosis: clinical symptomatology, pathophysiology, diagnostic approach, and therapeutic considerations." European archives of psychiatry and clinical neuroscience 270 (2020): 803-818.
- Al-Diwani, Adam, et al. "The psychopathology of NMDAR-antibody encephalitis in adults: a systematic review and phenotypic analysis of individual patient data." The Lancet Psychiatry 6.3 (2019): 235-246.
- Abboud, Hesham, et al. "Autoimmune encephalitis: proposed best practice recommendations for diagnosis and acute management." Journal of Neurology, Neurosurgery & Psychiatry 92.7 (2021): 757-768.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: This submission advances diversity, equity, and inclusion by addressing the diagnostic challenges of autoimmune encephalitis, particularly when presenting with psychiatric symptoms. Historically, psychiatric symptoms in medical settings can lead to misdiagnosis or delayed diagnosis, disproportionately affecting individuals with mental health concerns, often marginalized in healthcare. The Index-of-Suspicion framework proposed here aims to mitigate such disparities by providing a structured approach for timely and accurate diagnosis, thus promoting equitable access to appropriate care regardless of symptom presentation. This inclusive approach enhances clinical teaching, benefiting clinicians and learners in navigating complex diagnostic scenarios with sensitivity and efficacy.

