Catatonia
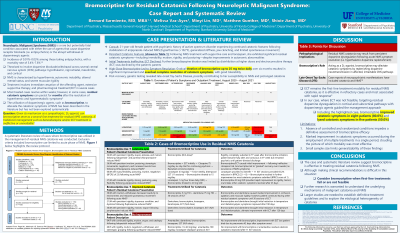
(019) Bromocriptine for Residual Catatonia Following Neuroleptic Malignant Syndrome: Case Report and Systematic Review

Bernard Sarmiento, MD (he/him/his)
Resident Physician
Massachusetts General Hospital / McLean Hospital Psychiatry Residency Program
Cambridge, Massachusetts- MV
Melissa Vaz-Ayes, B.S.
Medical Student
University of Florida College of Medicine
Gainesville, Florida - ML
Minyi Lin, MD
Resident
University of Florida
Gainesville, Florida 
Matthew Gunther, MD, MA (he/him/his)
Clinical Assistant Professor
Stanford University
Palo Alto, California- SJ
Shixie Jiang, M.D.
Assistant Professor
University of Florida College of Medicine
Gainesville, Florida
Presenting Author(s)
Co-Author(s)
Background/Significance:
Neuroleptic malignant syndrome (NMS) is a rare but potentially fatal iatrogenic syndrome characterized by hyperthermia, autonomic instability, altered mental status, and muscular rigidity (Strawn, 2007). While most cases of NMS resolve within days to weeks, residual catatonic symptoms in the absence of hyperthermic and hypermetabolic components can persist for months (Caroff, 2000). Although benzodiazepine and/or electroconvulsive therapy (ECT) are considered first-line treatment modalities for residual catatonia following NMS, there are situations where employment of such treatments are infeasible, contraindicated, and/or ineffective. The utilization of dopaminergic agents, such as bromocriptine, to lyse the catatonic symptoms of NMS has been described in the literature (Maia, 2021). The objective of this presentation is to present a case where bromocriptine was used to treat residual catatonia and to further delineate the role of bromocriptine in treating residual NMS catatonia through a systematic review.
Methods:
Following an illustrative case report where a patient’s residual catatonia was lysed with high-dose bromocriptine (25 mg twice daily), a systematic literature review of cases where bromocriptine was utilized in the management of residual NMS catatonia was conducted. Adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Group (PRISMA) 2020 guidelines, the databases of PubMed, Cochrane, PsychINFO, EBSCO, and OVID Medline were queried. Cases of bromocriptine use limited to the acute phase of NMS and cases without documentation of a residual catatonic state were excluded.
Results:
The systematic review initially identified 338 studies. 137 duplicate articles were identified by COVIDENCE and 76 irrelevant studies were excluded. 125 studies were assessed for eligibility, yielding seven manuscripts and nine total cases of bromocriptine use in residual NMS catatonia. Of these cases and including our own, bromocriptine use led to an improvement in catatonic symptoms in 80.0% of patients (8 out of 10) and helped to resolve catatonic symptoms in 50.0% of patients (5 out of 10).
Discussion:
The findings from this case report and accompanying systematic review suggest that bromocriptine is an effective, alternative treatment option for patients with residual catatonia following NMS. After considering benzodiazepine and/or ECT, employing bromocriptine is reasonable in addressing a patient’s residual catatonia. The potential efficacy of bromocriptine in treating this NMS complication may be attributed to persistent dopaminergic dysregulation in the mesocortical, mesolimbic, and nigrostriatal pathways of susceptible patients (Caroff, 2000).
Conclusion/Implications:
Based on this case report and accompanying systematic review, bromocriptine is an effective treatment option for patients with residual catatonia following NMS, particularly when first-line strategies such as benzodiazepine and/or ECT treatment have failed or are infeasible. Further research is needed to explore the pathophysiology and role of dopaminergic agents in NMS-associated complications.
References:
1. Strawn JR, Keck PE, Caroff SN. Neuroleptic Malignant Syndrome. AJP. 2007;164(6):870-876. doi:10.1176/ajp.2007.164.6.870
2. Caroff SN, Mann SC, Keck PEJ, Francis A. Residual Catatonic State Following Neuroleptic Malignant Syndrome. Journal of Clinical Psychopharmacology. 2000;20(2):257.
3. Maia A, Cotovio G, Barahona-Corrêa B, Oliveira-Maia AJ. Diagnosis and Treatment of Neuroleptic Malignant Syndrome in the Intensive Care Unit: A Case Report. Acta medica portuguesa. 2021;34(6):464-467. doi:10.20344/amp.13019
Presentation Eligibility: We expect to submit this research to the Journal of the Academy of Consultation-Liaison Psychiatry after April 1, 2024. To submit this research in the form of an oral or poster presentation, as well, will bring awareness to an alternative treatment modality for a rare complication of neuroleptic malignant syndrome.
Diversity, Equity, and Inclusion: Our topic includes a case report on an individual who suffered from a rare complication of neuroleptic malignant syndrome, that was unable to obtain first-line treatment in the form of ECT. The treatment of this patient's residual NMS catatonia may benefit patients in disadvantaged and/or historically marginalized populations who are unable to access traditional, first-line treatments due to health inequities.

