Collaborative and Integrated Care
(048) Analyzing the Impact of Crowding on Provider Attitudes: A Multidisciplinary Investigation in Emergency Medicine and Behavioral Health

Elizabeth Edwards, MD
Assistant Professor of Clinical Psychiatry
UIC College of Medicine Peoria Department of Psychiatry
Peoria, Illinois- BM
Bhavana Muppavarapu, n/a
Medical Student
University of Illinois College of Medicine Peoria
Peoria, Illinois - AP
Alexa Pronga, MD
Third Year Psychiatry Resident
University of Illinois College of Medicine- Peoria
Peoria, Illinois - AL
Andrew J. Lancia, MD, FACLP, DFAPA
Associate Professor
University of Illinois College of Medicine Peoria
Peoria, Illinois
Presenting Author(s)
Co-Author(s)
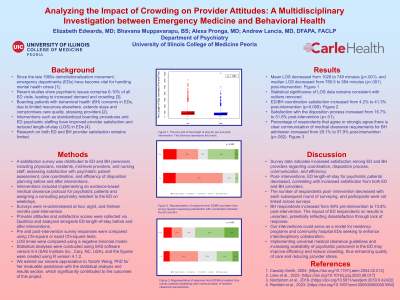
Background: Since the de-institutionalization movement in the late 1960s, emergency departments (EDs) have become crucial for managing crises in patients with mental health concerns [1]. Recent studies indicate that psychiatric illness accounts for 6-10% of all ED visits, leading to escalating demand and crowding issues [3]. Boarding patients with behavioral health (BH) complaints, due to limited resources elsewhere, prolongs ED stays and compromises care quality, adding stress for providers [2].
Methods: A provider satisfaction survey was distributed among ED and BH personnel, including physicians, residents, midlevel providers, and nursing staff, to assess satisfaction with the assessment of psychiatric patients, their care coordination, and the efficiency of disposition planning pre- and post-intervention. Interventions included implementing an evidence-based medical clearance protocol for psychiatric patients and assigning a consulting psychiatry resident to the ED on weekdays to assist with the assessment of presenting psychiatric concerns and disposition planning. Surveys are re-administered at one, three-, and six months post-intervention. Provider attitudes and satisfaction scores are being collected via Qualtrics and analyzed for satisfaction scores and length of stay (LOS) pre- and post-intervention.
Results: Preliminary results show that pre-implementation, only 4.2% were satisfied with BH-ED cooperation. Post-implementation, satisfaction rose to 41.2% (p=0.012). Dissatisfaction with behavioral health patient disposition significantly improved post-intervention, dropping from 58.1% to 16.7% (p< .001). Data collection is ongoing and further results are pending analysis.
Discussion: We hypothesize improved satisfaction in care coordination and decreased LOS following the staffing of a psychiatric resident and implementation of standardized medical clearance protocols in the ED. These anticipated improvements suggest enhanced collaboration between BH and ED departments, serving as a potential model for residency training programs and community hospital EDs aiming to improve interdisciplinary collaboration.
Implications: Universal medical clearance guidelines and increased availability of psychiatric personnel in the ED may enhance care efficiency and reduce crowding of psychiatric patients, ultimately improving care quality and provider satisfaction. These interventions have the potential to serve as a blueprint for similar settings and can be adapted to create collaborative-care environments that effectively reduce crowding among patients seeking care for psychiatric issues in the emergency department.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Universal medical clearance guidelines and increased availability of psychiatric personnel in the ED may not only enhance care efficiency and reduce crowding of psychiatric patients but also address disparities in access to mental health care among marginalized populations. These interventions hold promise in promoting diversity, equity, and inclusion by ensuring equitable access to quality mental health services, particularly for underserved communities reliant on EDs for psychiatric care.

