Catatonia
(034) The Medicine-Psychiatry Unit: After Dualism, Considering Catatonia from an Integrated Framework

Olivia Dahl, MD (she/her/hers)
resident physician
University Hospitals
Cleveland Heights, Ohio
Joaquin Santoy, MD
Resident
University Hospitals Cleveland Medical Center
Cleveland, Ohio- MM
Margaret Musso, MD
Resident
margaret.musso2@uhhospitals.org
Shaker Heights, Ohio 
Jennifer Brandstetter, MD, FAPA
Assistant Professor
University Hospitals Cleveland Medical Center
Cleveland, Ohio- SS
Syed Amir Z. Shah, MD
Assistant Professor
University Hospitals Cleveland Medical Center
Cleveland, Ohio
Presenting Author(s)
Co-Author(s)
Background/Significance:
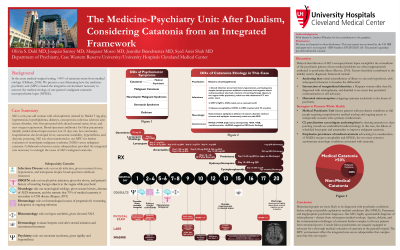
Catatonia is a prevalent neuropsychiatric syndrome historically relegated to the house of psychiatry, in spite of estimates that >50% of catatonia in the acute medical-surgical setting stems from medical etiology (Oldham, 2018). We present a case illustrating how the medicine-psychiatry unit (MPU) created the integrative environment necessary to uncover the medical etiology of one patient’s malignant catatonia: neuropsychiatric lupus (NPSLE).
Case:
A 66-year-old woman with schizophrenia, hypertension, hyperlipidemia, diabetes, osteoporosis, tuberous sclerosis and seizure disorder, MZ first presented with altered mental status, fever, and new oxygen requirement. Broad-spectrum antibiotics for lobar pneumonia initially yielded clinical improvement. When fever, autonomic instability, hyperreflexia, and dystonic posturing developed, she was transferred to our MPU for further evaluation of neuroleptic malignant syndrome (NMS) versus malignant catatonia. Collaboration between many subspecialties provided the integrated care necessary to correctly identify the etiology of MZ’s catatonia despite myriad possible explanations.
Subspecialty Consult Questions & Workup:
Infectious Disease: rule out occult infection, given recurrent fevers, hypotension, and leukopenia despite broad-spectrum antibiotic treatment
OBGYN: rule out occult pelvic infection, given the above and patient’s history of inserting foreign objects in the vagina while psychotic
Neurology: concern for neurological etiology, given seizure history, absence of AED treatment, and statistic that 70% of medical catatonia is secondary to CNS disease (Rogers, 2019).
Hematology: progressively worsening leukopenia
Rheumatology: concern for NPSLE, given elevated ANA
Dermatology: herpetic rash after steroid initiation
Psychiatry: rule out serotonin syndrome, given rigidity and hyperreflexia
Discussion:
MZ’s medical teams initially attributed MZ’s presentation to schizophrenia, and subsequent hesitation to broaden the diagnostic workup exemplified anchoring bias6. This is the conundrum of the psychiatric patient, whose medical problems are often prematurely written off as psychiatric illness (Reeves, 2010). Consulting psychiatrists played an important role in mitigating anchoring bias, drawing attention to clues pointing towards medical etiology: namely, the failure of scheduled lorazepam and amantadine to improve malignant catatonia significantly suggested that underlying etiology remained unremedied.
The MPU setting frames patients with psychiatric conditions as full people deserving of comprehensive medical workup-- in this case, by maintaining access to subspecialty consults to explore the two most common autoimmune neurologic conditions associated with catatonia, NMDA-receptor encephalitis and NPSLE. Offering access to interdisciplinary medical care in a psychiatrically qualified environment promotes whole health.
Conclusion:
Consult liaison psychiatrists are uniquely equipped to advocate for a thorough medical evaluation of catatonia in the general hospital. The MPU environment offers the integrated care across subspecialties that complex cases like this one require. References Oldham, MA. The Probability That Catatonia in the Hospital has a Medical Cause and the Relative Proportions of Its Causes: A Systematic Review. Psychosomatics. 2018;59(4):333-340. doi:10.1016/j.psym.2018.04.001 Rogers JP, Pollak TA, Blackman G, David AS. Catatonia and the immune system: a review. Lancet Psychiatry. 2019;6(7):620-630. doi:10.1016/S2215-0366(19)30190-7 Reeves RR, Parker JD, Loveless P, Burke RS, Hart RH. Unrecognized physical illness prompting psychiatric admission. Ann Clin Psychiatry. 2010 Aug;22(3):180-5.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Several marginalized identities intersected to dramatically increase MZ’s structural vulnerabilities: she carried a diagnosis of schizophrenia and she was Hispanic, older than 65, a woman, and, by the time she came into our care, so disabled by catatonia that she couldn’t communicate. Minoritized people are more likely to be diagnosed with psychiatric conditions before possible explanatory medical conditions (like NPSLE) have been ruled out, and psychiatric diagnoses detract from subsequent medical workups. Ageism, ableism, and the communication challenges of catatonia further conspire to divorce patients like MZ from structural power.

